The Lundquist Institute receives $2.6 million grant from U.S. Army Medical Research Acquisition Activity to develop wearable biosensors
The U.S. Army Medical Research Acquisition Activity (USAMRAA) has awarded The Lundquist Institute (TLI) a four-year grant totaling $2,623,234. The research project is led by Dr. Harry Rossiter, an investigator at TLI and Professor at the David Geffen School of Medicine at UCLA. The project aims to develop wearable multiplex biosensors to monitor exacerbation risk […]

The U.S. Army Medical Research Acquisition Activity (USAMRAA) has awarded The Lundquist Institute (TLI) a four-year grant totaling $2,623,234. The research project is led by Dr. Harry Rossiter, an investigator at TLI and Professor at the David Geffen School of Medicine at UCLA. The project aims to develop wearable multiplex biosensors to monitor exacerbation risk in chronic obstructive pulmonary disease (COPD).

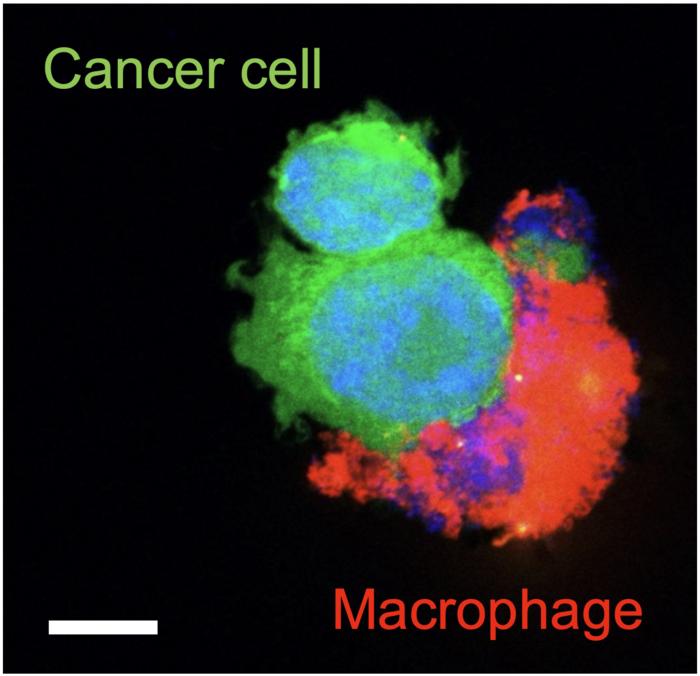
Credit: The Lundquist Institute for Biomedical Innovation at Harbor-UCLA Medical Center
The U.S. Army Medical Research Acquisition Activity (USAMRAA) has awarded The Lundquist Institute (TLI) a four-year grant totaling $2,623,234. The research project is led by Dr. Harry Rossiter, an investigator at TLI and Professor at the David Geffen School of Medicine at UCLA. The project aims to develop wearable multiplex biosensors to monitor exacerbation risk in chronic obstructive pulmonary disease (COPD).
COPD affects approximately 16 million Americans and is the third leading cause of death globally. Acute exacerbations of COPD (AECOPD), typically caused by a lung infection, are associated with accelerated progression of COPD and represent the greatest burden of COPD to patients and healthcare. Patients with AECOPD have increased breathlessness, typically reported several days after the initial infection, and may require treatment with antibiotics and/or hospitalization.
The prediction of AECOPD is complex. Evidence of the early response to infection, before the onset of symptoms, is present in blood in the form of inflammatory signaling molecules. The collaborative team from the Lundquist Institute (led by Harry Rossiter, PhD) and Caltech (led by Wei Gao, PhD) have already developed a wearable nanoengineered biosensor that allows real-time, non-invasive analysis of the inflammatory signaling molecule C-reactive protein (CRP) in sweat, that is associated with the blood-borne response. Building on this development, their new research will identify molecules in sweat that predict future AECOPD, paving the way for real-time, on body, monitoring without the need for repeated blood samples.
“Our ultimate goal is to develop a wearable system to preempt AECOPD, providing an early warning system to move treatment earlier in the exacerbation process and thereby reduce patient morbidity, mortality, hospitalization, and healthcare utilization,” said Dr. Rossiter. “The proposed sensor has the potential to not only revolutionize COPD management but also to impact healthcare by incorporating wearable electronics into chronic disease management.”
“In partnership with Dr. Harry Rossiter and The Lundquist Institute, our team at Caltech is advancing medical technology with wearable biosensors. Our aim with this project is to transform chronic disease management and push healthcare towards continuous, non-invasive monitoring for better health,” said Dr. Wei Gao.
What's Your Reaction?