Shattering the Silence: Investigating Men’s Bone Fractures
In recent years, osteoporosis has increasingly been recognized as a silent yet pervasive health threat, predominantly among women. However, a new wave of scientific attention is now turning toward a less discussed but equally critical demographic: men. Osteoporosis, characterized by progressive loss of bone density and structural degradation of bone tissue, presents a hidden risk […]


In recent years, osteoporosis has increasingly been recognized as a silent yet pervasive health threat, predominantly among women. However, a new wave of scientific attention is now turning toward a less discussed but equally critical demographic: men. Osteoporosis, characterized by progressive loss of bone density and structural degradation of bone tissue, presents a hidden risk that many men underestimate or overlook entirely. This under-recognition stems partly from the misconception that osteoporosis is primarily a woman’s disease, leaving a staggering number of men vulnerable to fractures and debilitating bone injuries without adequate preventive measures or treatment.
At the age of 40, for example, individuals like Brad Barbin—who once faced weakening bones—have now adopted rigorous physical routines, walking four to five miles daily to combat the onset of osteoporosis. Such efforts highlight the emerging understanding that maintaining bone health through continuous physical activity, particularly resistance training, is vital in preserving skeletal strength into middle and older ages. Without these preventative actions, men risk losing bone mass at an alarming rate of up to 3% per year starting in their fourth decade of life, a statistic that underscores the urgency of early intervention.
A survey commissioned by The Ohio State University Wexner Medical Center exposes a concerning knowledge gap: only 1% of men express concern regarding their bone density. This apathy contrasts sharply with men’s greater awareness of other health risks, such as cancer and cardiovascular disease, which dominate their health priorities. Yet, the consequences of undiagnosed and untreated osteoporosis in men can be catastrophic. Spinal and pelvic fractures, frequently treated by interventional radiologists like Dr. Paul Lewis, often mark the first clinical manifestations of this silent disease, heralding a sudden decline in mobility, independence, and overall quality of life.
.adsslot_QvKGEiIbce{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_QvKGEiIbce{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_QvKGEiIbce{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
Osteoporosis in men tends to progress without overt symptoms until a fracture occurs. This “noise” that clinicians warn about manifests itself devastatingly through breaks caused by minimal trauma, often from simple falls. The pathophysiology involves the gradual loss of bone mineral density (BMD), microarchitectural decay, and impaired bone remodeling. Osteopenia—the stage of reduced bone mass prior to full osteoporosis—affects an even larger subset of men, signifying a prelude to more severe bone fragility if unaddressed. The National Spine Health Foundation estimates that approximately 2 million men suffer from osteoporosis, with an additional 16 million experiencing osteopenia, calling for heightened vigilance within this population.
The hormonal milieu plays a crucial role in bone metabolism, especially the diminishing levels of testosterone that accompany aging in men. Testosterone supports bone formation by stimulating osteoblast activity and inhibiting osteoclast-mediated bone resorption. Declining testosterone, therefore, disrupts this balance, favoring bone loss. The intersection of endocrine aging and skeletal deterioration illuminates why men must begin conversations about bone health with healthcare providers as early as age 30, well before the physical signs of osteoporosis emerge.
Preventive strategies are multifactorial and emphasize lifestyle modifications. Resistance training exercises are particularly effective in mechanically stimulating bone formation and slowing resorption. Additionally, nutritional optimization—including adequate intake of calcium, vitamin D, and protein—forms a cornerstone of preventive care. Smoking cessation and moderation of alcohol consumption further mitigate risk factors associated with accelerated bone loss. These interventions aim to maintain skeletal integrity by reinforcing bone mass and minimizing the progression of porosity and brittleness intrinsic to osteoporosis.
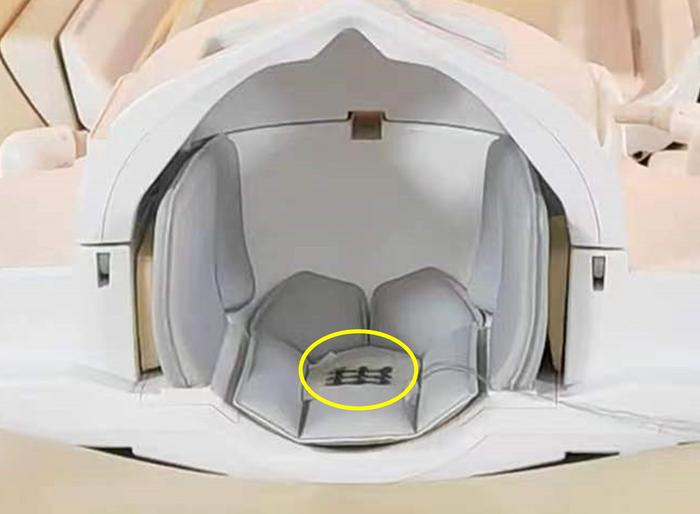
When fractures occur, especially in the vertebrae, interventional radiology offers innovative and minimally invasive treatment modalities such as kyphoplasty and vertebroplasty. Kyphoplasty involves the insertion and inflation of a small balloon within the fractured vertebral body to create a cavity, which is subsequently filled with polymethyl methacrylate (PMMA) bone cement. This procedure not only stabilizes the fracture but also aims to restore vertebral body height and spinal alignment, thereby alleviating pain and improving patient mobility. Vertebroplasty follows a similar principle but omits balloon inflation, with direct cement injection into the collapsed vertebra for immediate stabilization and analgesic effect.
Both procedures are performed under sedation with real-time fluoroscopic guidance, offering significant advantages over open surgical interventions. These minimally invasive options facilitate rapid recovery, minimal downtime, and reduced procedural risk, allowing patients to regain function swiftly and maintain independence. Such advancements underscore the evolving landscape of osteoporosis management, where symptom control complements preventive care to improve long-term outcomes.
The broader implications of untreated osteoporosis extend beyond individual skeletal health. Fractures can result in prolonged immobility, increased risk of secondary complications such as deep vein thrombosis, pneumonia, and muscle atrophy, and heightened mortality, particularly among older adults. By addressing osteoporosis early, healthcare providers aim not only to preserve bone strength but to enhance overall physical activity, diminish isolation caused by pain and disability, and promote sustained quality of life.
The recent survey conducted by SSRS between May 2 and May 5, 2025, sampled over 1,000 U.S. adults, highlighting a critical need for educational initiatives targeting men. Despite high concern for cancer and heart disease, bone health remains grossly underappreciated. Public health campaigns aligning with Men’s Health Awareness Month aim to bridge this awareness gap by disseminating crucial information about bone density testing, lifestyle interventions, and the availability of effective treatments.
This growing body of evidence demands a paradigm shift in how male osteoporosis is perceived and managed. Integrating bone health into routine preventive screenings and health discussions is essential for reducing the incidence of fractures and their consequential disability. As men become more proactive through early screening, informed lifestyle choices, and timely interventions, the silent threat of osteoporosis can be transformed into a manageable, controllable condition, improving longevity and quality of life worldwide.
Subject of Research: Osteoporosis in men, bone density loss, interventional radiology treatments
Article Title: Silent Threat: Unveiling the Hidden Risk of Osteoporosis Among Men
News Publication Date: June 2025
Web References:
The Ohio State University Wexner Medical Center: https://wexnermedical.osu.edu/
National Spine Health Foundation: https://spinehealth.org/osteoporosis-in-men/
Image Credits: The Ohio State University Wexner Medical Center
Keywords: Bones, Osteoporosis, Bone Diseases, Preventive Medicine, Physical Exercise, Human Physiology, Health Care, Radiology
Tags: aging and skeletal healthbone density loss in menearly intervention for osteoporosismen’s health awarenessmen’s vulnerability to fracturesmisconceptions about osteoporosisosteoporosis awareness campaignsosteoporosis in menphysical activity for bone healthprevention of bone fracturesresistance training benefitssilent osteoporosis risk
What's Your Reaction?