How popular steroids could mess up some cancer treatments
Immunotherapy is among the newest and most potent weapons against cancer. It prompts the immune system to recognize tumors as intruders in the body and attack. But not all patients respond well to immunotherapy. Why? Scientists aren’t always sure. Credit: Janowitz lab/Cold Spring Harbor Laboratory Immunotherapy is among the newest and most potent weapons against […]

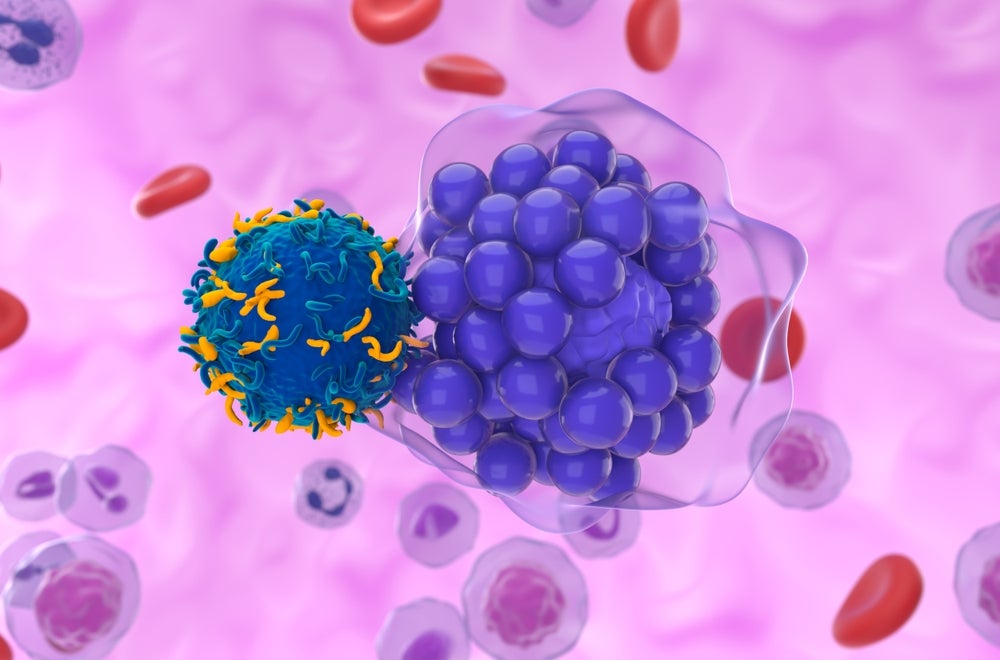
Immunotherapy is among the newest and most potent weapons against cancer. It prompts the immune system to recognize tumors as intruders in the body and attack. But not all patients respond well to immunotherapy. Why? Scientists aren’t always sure.

Credit: Janowitz lab/Cold Spring Harbor Laboratory
Immunotherapy is among the newest and most potent weapons against cancer. It prompts the immune system to recognize tumors as intruders in the body and attack. But not all patients respond well to immunotherapy. Why? Scientists aren’t always sure.
Sometimes, immunotherapy patients experience side effects that steroids called glucocorticoids (GCs) can treat. GCs are often used to regulate the immune response in conditions such as asthma, Crohn’s disease, and even COVID-19. Yet just how they work is also a mystery.
Now, Cold Spring Harbor Laboratory (CSHL) researchers may be closer to answering both questions. Their new research indicates GCs may indirectly lead to some immunotherapy treatment failures by driving the production of a protein called Cystatin C (CyC). Higher levels of CyC are linked to poorer outcomes of this type of therapy.
CSHL Assistant Professor Tobias Janowitz says, “GCs are very powerful suppressors of immunity and are consequently used to treat autoimmunity,” which is when the immune system attacks healthy cells. “We’ve previously shown that GCs can also break cancer immunotherapy. Now, here’s perhaps a clue into how they’re doing it.”
Janowitz’s lab studies the whole-body response to cancer. For this study, he and a Ph.D. student in his lab, physician-turned-researcher Sam Kleeman, teamed with a third CSHL scientist, Assistant Professor Hannah Meyer, an expert in quantitative biology. Together, they analyzed a massive genetic dataset from the UK Biobank. How massive? Almost 500,000 volunteers, including patients with cancer. Kleeman also reached out to researchers overseas to gather even more patient data.
The scientists found that patients who were more likely to produce CyC in response to GCs had a worse overall survival rate. These patients were also less likely to benefit from treatment. This suggests CyC production within a tumor may contribute to the failure of cancer immunotherapy.
To confirm CyC’s connection with cancer, the researchers turned to good old-fashioned lab work. In mice, they deleted a CyC-producing gene so it was no longer present in cancer cells. They found that tumors without CyC grew slower.
“It’s really powerful to come at this from multiple angles and support the findings through many approaches,” Meyer says. “Clever genetic models gave us some indication of which experiments to design to help us answer the question of what this molecule does.”
Janowitz says he plans to continue studying CyC. He hopes this could greatly help future patients.
“The research has given me an impetus to find out more about the function of this molecule, specifically in the context of cancer immunotherapy,” he says. “Perhaps its function can be targeted to enhance the success of cancer immunotherapy.”
Journal
Cell Genomics
DOI
10.1016/j.xgen.2023.100347
Article Title
Cystatin C is glucocorticoid-responsive, directs recruitment of Trem2+ macrophages and predicts failure of cancer immunotherapy
Article Publication Date
23-Jun-2023
What's Your Reaction?