Upgraded tumor model optimizes search for cancer therapies
HOUSTON – (March 20, 2023) – Tumor cells won’t show their true selves in a petri dish, isolated from other cells. Credit: (Photo by Gustavo Raskosky/Rice University) HOUSTON – (March 20, 2023) – Tumor cells won’t show their true selves in a petri dish, isolated from other cells. To find out how they really behave, […]

HOUSTON – (March 20, 2023) – Tumor cells won’t show their true selves in a petri dish, isolated from other cells.

Credit: (Photo by Gustavo Raskosky/Rice University)
HOUSTON – (March 20, 2023) – Tumor cells won’t show their true selves in a petri dish, isolated from other cells.
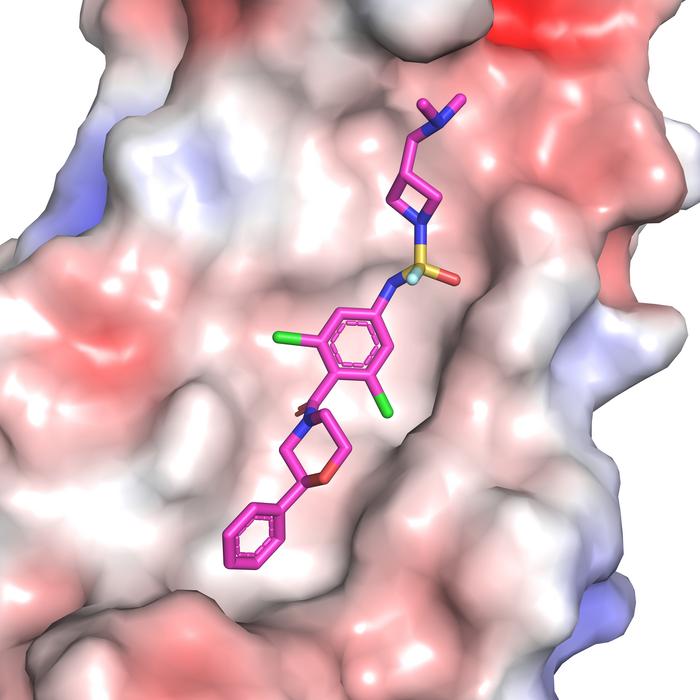
To find out how they really behave, Rice University researchers developed an upgraded tumor model that houses osteosarcoma cells beside immune cells known as macrophages inside a three-dimensional structure engineered to mimic bone. Using the model, bioengineer Antonios Mikos and collaborators found that the body’s immune response can make tumor cells more resistant to chemotherapy.
The study, which is published in Biomaterials, sheds light on why some cancer drugs that appear to be good candidates in the lab do not perform as well as expected in actual patients. It underscores weaknesses in traditional tumor modeling and points the way toward more effective cancer therapies.
“Existing tumor models used to test drug performance do not mimic the actual environment in the human body closely enough,” Mikos said. “We are trying to create an environment for the experiment that is closer to what is happening in the organism of actual patients. Having such an environment will allow us to test multiple drugs in a time- and cost-effective way.”
Mikos’ lab had shown in previous work that cancer cells are sensitive to the mechanical properties of their substrate.
“Typically, cells would be grown on a flat surface, like in a petri dish,” said Letitia Chim, who recently earned a doctorate at Rice and was the lead author on the study. “If you use a microscope to look at the disc-shaped scaffolds we developed, you can see that they are made up of these fiber structures on the scale of what cells would recognize. The cells can sense that this substrate is three-dimensional instead of flat — closer to what bone structure is like.”
The scaffolds are made from two different materials: a very stiff synthetic polymer and gelatin. By changing the ratio of the materials, researchers can control the overall stiffness of the fibers.
“What is new here and very revealing is that we added the next level of complexity — the immune cells that are part of the tumor microenvironment — and looked at how the combination of the mechanical responsiveness of the substrate and the presence of other cells factors into tumor development and behavior,” Mikos said.
“In a tumor, you don’t only have the cancer cells, you have other cells that are sending out signals that can affect how the cancer cells will respond to treatment,” Chim said.
Researchers found that increased inflammation caused by macrophages reduced the effectiveness of doxorubicin, one of the chemotherapeutic agents used to treat osteosarcoma, which is the most common form of bone cancer.
“We were interested in tumor-associated macrophages because they can make up to 50% of the tumor,” Chim said. “Tumors have sometimes been described as wounds that never heal, and that’s partly due to the macrophages sending out wound-healing signals. In normal tissue that works well, but it can also benefit the tumor.”
Preclinical models that mimic tumors more accurately can help researchers identify which therapies are most effective in a given context.
“This is going to be useful in order to design therapeutics that target not only the cancer cells but also the immune cells, or that trigger the immune cells to essentially change their function,” Mikos said.
“A major objective of our research is to develop personalized testing systems or platforms where the characteristics of the patient’s tumor are used to find a therapeutic model that works best for them,” Chim said. “I would say that’s the personalized medicine vision of the future: being able to answer the question, are there particular targeted treatments that work well for this patient?
“Osteosarcoma is a rare disease that often gets overlooked. It’s also a really complicated disease that shows up differently in every single patient. This is another reason why it would ultimately be great if we can develop a personalized medicine approach for treating osteosarcoma.”
“The tumor microenvironment clearly plays an important role in how disease progression and treatment unfold,” Mikos said. “That is why we strive to develop an optimal level of complexity that captures the bigger picture of what actually happens inside a live organism.”
Rice assistant professor of bioengineering and biosciences Caleb Bashor and undergraduate alum Isabelle Williams are co-authors on the study.
Mikos is Rice’s Louis Calder Professor of Bioengineering and Chemical and Biomolecular Engineering and director of the Center for Excellence in Tissue Engineering and the J.W. Cox Laboratory for Biomedical Engineering.
The National Institutes of Health (R01CA180279, P41EB023833) funded the research.
-30-
This release can be found online at news.rice.edu.
Follow Rice News and Media Relations via Twitter @RiceUNews.
Peer-reviewed paper:
Tumor-associated macrophages induce inflammation and drug resistance in a mechanically tunable engineered model of osteosarcoma | Biomaterials | DOI: 10.1016/j.biomaterials.2023.122076
Authors: Letitia Chim, Isabelle Williams, Caleb Bashor and Antonios Mikos
https://doi.org/10.1016/j.biomaterials.2023.122076
Image downloads:
https://news-network.rice.edu/news/files/2023/03/2303_Bashor_Mikos_Chim_LG.jpg
CAPTION: Study co-authors (from left) Caleb Bashor, Antonios Mikos and Letitia Chim. (Photo by Gustavo Raskosky/Rice University)
https://news-network.rice.edu/news/files/2023/03/2303_Chim_LG.jpg
CAPTION: Letitia Chim, who recently earned a doctorate at Rice, is a lead author on the study. (Photo by Gustavo Raskosky/Rice University)
https://news-network.rice.edu/news/files/2023/03/2303_Mikos_sample_LG-1.jpg
CAPTION: The disc-shaped 3D scaffolds used to model the tumor microenvironment mimics bone structure and texture. (Photo by Gustavo Raskosky/Rice University)
Related stories:
Mikos wins Jensen Tissue Engineering Award:
https://news.rice.edu/news/2022/mikos-wins-jensen-tissue-engineering-award
Links:
Bashor lab: http://bashorlab.rice.edu/index_small.html
Mikos lab: http://mikoslab.rice.edu/
Bioscience Research Collaborative (BRC): https://brc.rice.edu/
Biomaterials Lab: https://research.rice.edu/bml/
Rice Department of Bioengineering: https://bioengineering.rice.edu/
Located on a 300-acre forested campus in Houston, Rice University is consistently ranked among the nation’s top 20 universities by U.S. News & World Report. Rice has highly respected schools of Architecture, Business, Continuing Studies, Engineering, Humanities, Music, Natural Sciences and Social Sciences and is home to the Baker Institute for Public Policy. With 4,552 undergraduates and 3,998 graduate students, Rice’s undergraduate student-to-faculty ratio is just under 6-to-1. Its residential college system builds close-knit communities and lifelong friendships, just one reason why Rice is ranked No. 1 for lots of race/class interaction and No. 1 for quality of life by the Princeton Review. Rice is also rated as a best value among private universities by Kiplinger’s Personal Finance.
Journal
Biomaterials
DOI
10.1016/j.biomaterials.2023.122076
Method of Research
Experimental study
Subject of Research
Cells
Article Title
Tumor-associated macrophages induce inflammation and drug resistance in a mechanically tunable engineered model of osteosarcoma
Article Publication Date
7-Mar-2023
COI Statement
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
What's Your Reaction?