Organ Preservation in Lung Cancer: Extended Sleeve Lobectomy Following Neoadjuvant Immunochemotherapy Emerges as Optimal Strategy for Centrally Located NSCLC
In a groundbreaking advancement poised to reshape surgical options for centrally located non-small cell lung cancer (NSCLC), a new retrospective study published in the April 2025 issue of Annals of Thoracic Surgery sheds illuminating light on the safety and efficacy of extended sleeve lobectomy (ESL) following neoadjuvant immunochemotherapy. Spearheaded by Professors Jianxing He and Shuben […]


In a groundbreaking advancement poised to reshape surgical options for centrally located non-small cell lung cancer (NSCLC), a new retrospective study published in the April 2025 issue of Annals of Thoracic Surgery sheds illuminating light on the safety and efficacy of extended sleeve lobectomy (ESL) following neoadjuvant immunochemotherapy. Spearheaded by Professors Jianxing He and Shuben Li from the First Affiliated Hospital of Guangzhou Medical University, this comprehensive analysis addresses a critical gap in thoracic oncology and surgical practice, offering hope for patients traditionally facing pneumonectomy (PN), a procedure long associated with substantial morbidity and diminished postoperative lung function.
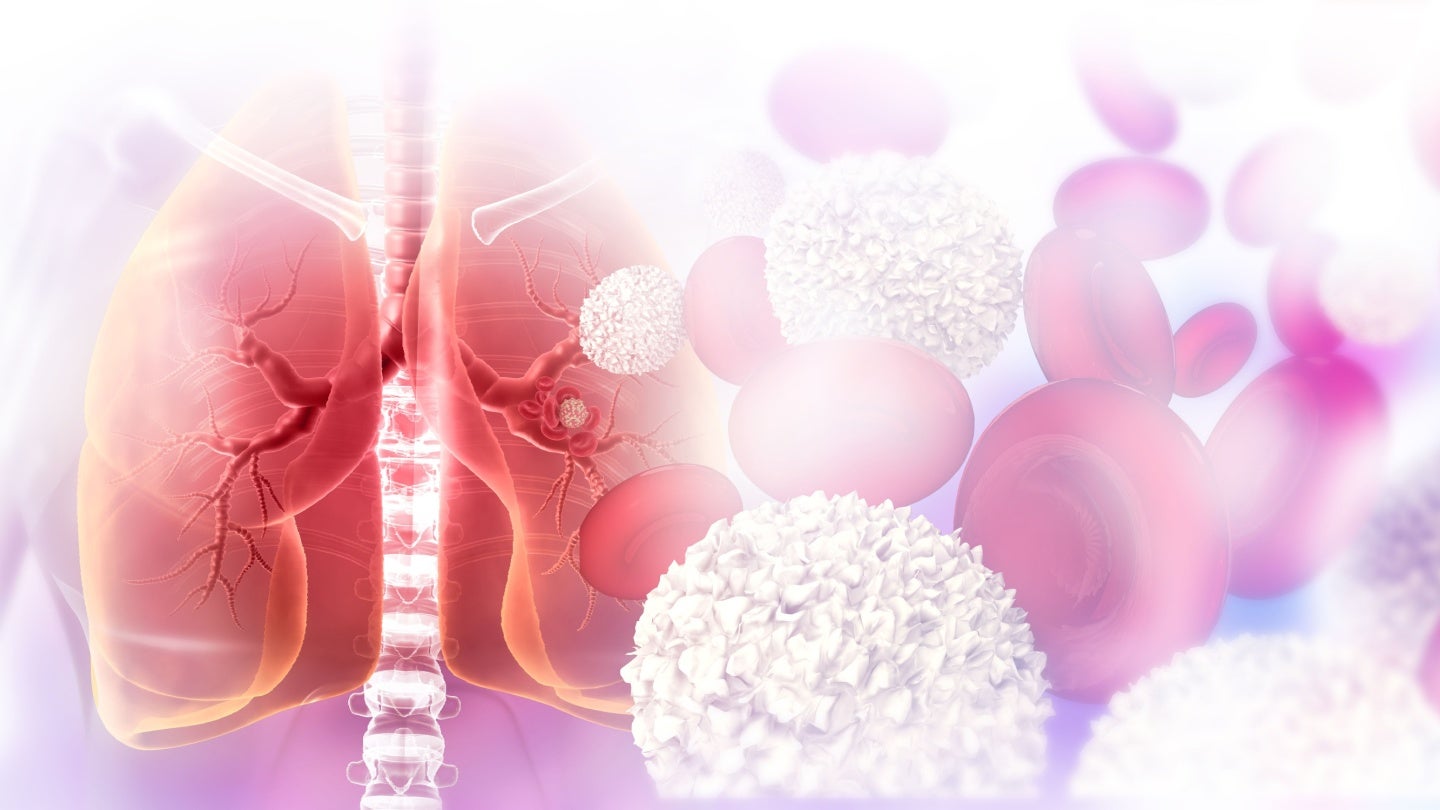
NSCLC, particularly when centrally located, presents formidable challenges due to its aggressive nature and anatomical proximity to vital bronchovascular structures. The conventional mainstay treatment—pneumonectomy—involves removal of an entire lung but carries significant risks. High rates of morbidity and mortality, along with drastic reductions in pulmonary reserve, frequently compromise patients’ quality of life and limit opportunities for additional adjuvant therapies. As such, the thoracic surgery community has increasingly sought lung-parenchyma-preserving interventions, with bronchoplasty techniques and sleeve lobectomy emerging as promising alternatives that balance oncologic control with functional preservation.
Sleeve lobectomy (SL), which entails resection of the lung lobe along with a segment of the bronchus and subsequent bronchial reconstruction, has demonstrated superior survival and postoperative pulmonary function compared to pneumonectomy. However, when the extent of tumor involvement precludes a standard sleeve lobectomy (SSL), surgical options become severely constrained. Extended sleeve lobectomy (ESL)—a more complex procedure involving resection and reconstruction of additional airway and vascular structures—has been proposed to circumvent the need for pneumonectomy, yet its safety profile, particularly after neoadjuvant immunochemotherapy, has remained uncertain.
.adsslot_a9f8pRkd5B{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_a9f8pRkd5B{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_a9f8pRkd5B{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
Neoadjuvant immunochemotherapy, combining immune checkpoint inhibitors with chemotherapy agents prior to surgery, has transformed the treatment landscape for NSCLC by enhancing tumor downstaging and potentially improving long-term survival. While the safety and feasibility of SSL in the context of this novel systemic approach have been documented, ESL’s role post-immunochemotherapy has remained largely unexplored until now. This study addresses that knowledge gap by meticulously analyzing outcomes of ESL in patients treated with neoadjuvant immunochemotherapy, comparing morbidity, oncological radicality, and survival against those undergoing SSL or PN.
The investigators retrospectively reviewed 94 cases of centrally located NSCLC patients who received neoadjuvant immunochemotherapy, followed by either pneumonectomy, ESL, or SSL. Remarkably, complete R0 resections—indicating no microscopic residual tumor—were achieved in 95.7% of these cases. The R0 resection rates were comparably high across groups: 94.4% in ESL, 97.6% in SSL, and 94.1% in PN, underscoring the oncological rigor of ESL despite its technical complexity. This finding challenges skepticism that ESL may compromise surgical radicality when compared to more conventional approaches.
In terms of postoperative complications, the overall rate was relatively contained at 18.1%. While patients who underwent pneumonectomy experienced a higher complication rate of 32.4%, no statistically significant difference was detected between ESL and PN groups. Importantly, the ESL group’s morbidity rates closely paralleled those seen with the technically less demanding SSL, supporting ESL’s safety in adept hands following neoadjuvant immunochemotherapy. These results defy entrenched assumptions that extended resection and reconstruction inherently lead to prohibitive perioperative risks.
Long-term outcomes further bolster ESL’s standing as a viable alternative. Kaplan–Meier survival analyses revealed no significant difference in event-free survival between ESL and SSL, indicating that the extended surgical approach does not compromise prognosis. Strikingly, patients undergoing ESL demonstrated a statistically significant advantage in event-free survival compared to those receiving pneumonectomy (P=0.04). Such data suggest that ESL not only preserves lung tissue and function but may also confer improved oncological outcomes in this high-risk population.
The clinical ramifications of these findings are profound. ESL after neoadjuvant immunochemotherapy presents a technically complex but feasible and oncologically sound option that mitigates the devastating functional losses associated with pneumonectomy. By preserving greater lung parenchyma, ESL can maintain higher pulmonary reserves, reduce perioperative morbidity, and facilitate access to subsequent adjuvant therapies—elements crucial for enhancing patient quality of life and survival. This approach epitomizes precision surgery in thoracic oncology, aligning therapeutic aggressiveness with the imperative to safeguard physiological function.
Furthermore, the study underscores the importance of multidisciplinary collaboration, integrating cutting-edge systemic therapies with advanced surgical techniques. The interplay between neoadjuvant immunochemotherapy’s tumor-shrinking effects and ESL’s parenchymal-sparing strategy exemplifies a paradigm shift. It signals a move away from one-size-fits-all pneumonectomy toward individualized, multimodal treatments tailored to tumor extent, patient fitness, and functional status.
Despite these encouraging results, ESL remains a technically demanding procedure necessitating high surgical expertise and careful patient selection. Thorough preoperative assessment—including detailed imaging and bronchoscopic evaluation—is paramount to delineate tumor boundaries and plan airway reconstructions. Likewise, perioperative management must anticipate potential complications inherent to extensive bronchovascular reconstructions, necessitating experienced surgical teams and comprehensive postoperative care.
Critically, this study’s findings advocate for broadening the surgical repertoire available to thoracic surgeons treating central NSCLC. Adoption of ESL post-neoadjuvant immunochemotherapy promises to reduce reliance on pneumonectomy, potentially translating into better postoperative function and survival outcomes for a patient subset historically tethered to more radical resections. The implications extend beyond individual patient benefit, potentially reshaping clinical guidelines and influencing training paradigms within thoracic surgery.
This evidence further highlights the transformative role neoadjuvant immunochemotherapy plays in optimizing surgical candidacy and outcomes. By effectively downstaging tumors, this systemic approach increases the feasibility of lung-sparing techniques like ESL. It reflects a new frontier in NSCLC management, where the integration of immunotherapy and advanced surgical modalities converge to improve both oncologic control and patient-centered outcomes.
In summary, the study by He, Li, and colleagues marks a milestone in thoracic oncology, establishing extended sleeve lobectomy following neoadjuvant immunochemotherapy as a safe, effective, and function-preserving surgical option for centrally located NSCLC. These findings invite thoracic surgeons worldwide to consider ESL as a potent alternative to pneumonectomy, particularly when standard sleeve lobectomy is insufficient for achieving complete tumor removal. As research in immunotherapy and surgical techniques evolves, such multidisciplinary approaches will be pivotal in redefining standards of care for lung cancer, ultimately translating into better survival and quality of life for patients.
Subject of Research: People
Article Title: Extended Sleeve Lobectomy After Neoadjuvant Immunochemotherapy for Centrally Located Non-small Cell Lung Cancer
News Publication Date: 9-Apr-2025
Web References: http://dx.doi.org/10.1016/j.athoracsur.2025.03.033
Keywords: Lung cancer, Clinical studies
Tags: bronchoplasty techniques in lung surgerycentrally located NSCLC treatment optionsextended sleeve lobectomy in NSCLClung-parenchyma-preserving interventionsminimally invasive lung cancer proceduresneoadjuvant immunochemotherapy safetyOrgan preservation in lung cancerpatient quality of life after lung surgerypneumonectomy alternatives for lung cancerretrospective study on lung cancer surgerysurgical outcomes in lung cancerthoracic oncology advancements
What's Your Reaction?