Gasdermin E Drives Pyroptosis Resistance in Glioblastoma
In a groundbreaking study poised to redefine our understanding of glioblastoma biology, researchers have uncovered a paradoxical role of Gasdermin E (GSDME) in this aggressive brain cancer. Traditionally recognized as a crucial mediator of pyroptosis—a highly inflammatory and lytic form of programmed cell death—GSDME has now been found to contribute to glioblastoma’s notorious resistance to […]


In a groundbreaking study poised to redefine our understanding of glioblastoma biology, researchers have uncovered a paradoxical role of Gasdermin E (GSDME) in this aggressive brain cancer. Traditionally recognized as a crucial mediator of pyroptosis—a highly inflammatory and lytic form of programmed cell death—GSDME has now been found to contribute to glioblastoma’s notorious resistance to pyroptosis, simultaneously promoting tumor progression. This unexpected duality challenges existing paradigms around cell death pathways in cancer and opens novel avenues for therapeutic intervention.
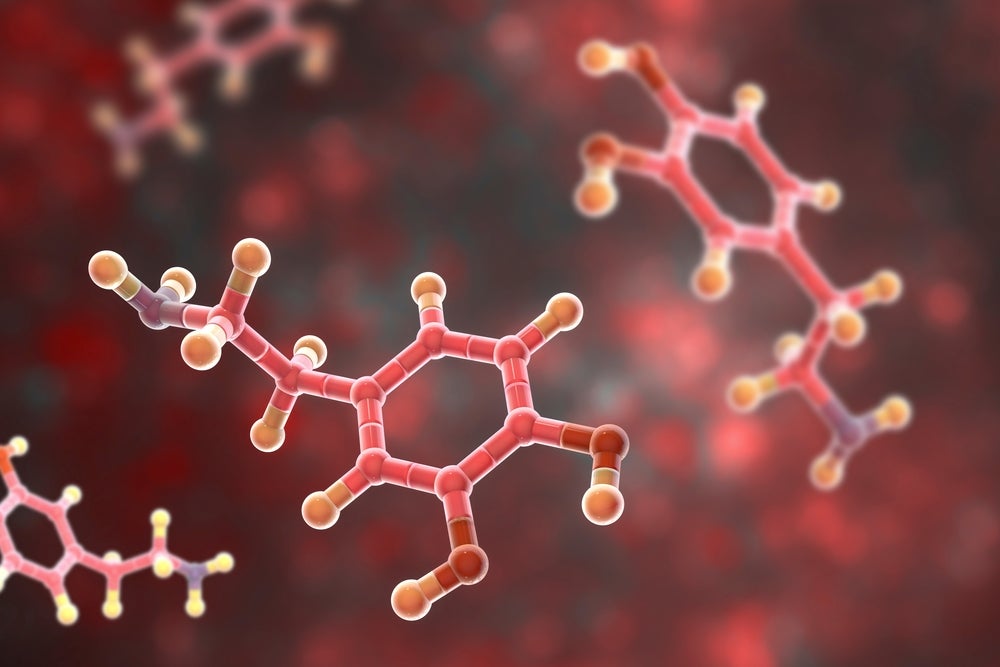
Glioblastoma remains one of the deadliest and most refractory tumors, with median survival barely exceeding a year despite aggressive treatments. Tumor heterogeneity, adaptive resistance mechanisms, and a highly immunosuppressive microenvironment contribute to its resilience. Recent cancer research has increasingly focused on exploiting cell death modalities such as pyroptosis to overcome resistance and sensitize tumors to therapy. GSDME stands out among gasdermin family members for its canonical role as a pyroptotic executor, typically activated downstream of caspase-3, enabling membrane pore formation and consequent inflammatory cell lysis.
The newly published work, led by Solel et al., ventures deep into how glioblastoma cells manipulate GSDME function to evade pyroptotic demise. The study provides compelling evidence that glioblastoma cells not only resist GSDME-mediated pyroptosis but paradoxically utilize GSDME to enhance malignant behaviors including proliferation, migration, and immune evasion. This reshapes GSDME from a straightforward tumor suppressor into a multifaceted contributor to tumor fitness—a revelation with profound implications for therapeutic strategies targeting programmed cell death pathways.
.adsslot_TfpQ2yVi60{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_TfpQ2yVi60{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_TfpQ2yVi60{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
Mechanistically, the researchers demonstrated that glioblastoma cells exhibit altered post-translational modifications and spatial distribution of GSDME, preventing canonical cleavage events that would trigger pyroptosis. Instead, GSDME predominantly localizes in subcellular compartments associated with tumorigenic signaling cascades, maintaining cell viability while fostering oncogenic phenotypes. This subversion of a conventional death effector underscores the ingenuity of glioblastoma’s survival arsenal and suggests that attempts to pharmacologically augment GSDME-induced pyroptosis could face unexpected pitfalls.
The interplay between GSDME and the tumor microenvironment also emerged as a critical axis shaping glioblastoma progression. Resistant glioblastoma cells, through GSDME-dependent mechanisms, appear to modulate immune cell recruitment and activation, contributing to the immune-escape characteristic of these tumors. By dampening inflammatory signals typically unleashed during pyroptosis, glioblastoma modifies immune landscape to its advantage, fostering an environment conducive to tumor growth and therapy resistance.
Importantly, the study utilises a combination of in vitro glioblastoma models, patient-derived cells, and in vivo murine systems to validate these findings. This multifaceted approach ensures robustness of the conclusions and provides a translational backbone emphasizing the clinical relevance of targeting GSDME pathways. The authors discuss the nuance required in therapeutic design, suggesting that overcoming GSDME’s tumor-promoting functions may necessitate interventions beyond simple activation of pyroptosis triggers.
The revelation that GSDME functions diverge dramatically between cancer types adds an additional layer of complexity. While in several cancers GSDME activation corresponds with enhanced cell death and better clinical outcomes, glioblastoma inverts this relationship. Such context-dependent functional plasticity mandates cancer-specific explorations before generalizing gasdermin-targeted approaches, highlighting the need for precision oncology frameworks tailored to molecular and microenvironmental tumor landscapes.
In describing the molecular underpinnings, the authors identify critical post-translational modifiers, including phosphorylation sites and interacting partners, that attenuate GSDME’s pore-forming activity in glioblastoma cells. These modifications appear to be orchestrated by oncogenic signaling nodes frequently dysregulated in glioblastoma, such as the PI3K/AKT and MAPK pathways. This integrative signaling crosstalk positions GSDME as a nexus where cell death resistance and pro-tumoral signaling converge, pinpointing novel targets for combination therapies.
Furthermore, the study delves into how GSDME influences cellular metabolism and stress response pathways. Glioblastoma cells leverage GSDME to sustain metabolic flexibility in hostile microenvironments characterized by hypoxia and nutrient deprivation. This metabolic support role stands in stark contrast to the enzyme’s canonical pyroptotic function and demonstrates the evolutionary adaptability of cancer cells to repurpose death effectors for survival advantages.
Equally striking is the finding that GSDME expression levels correlate with poor prognosis in glioblastoma patients, as shown through rigorous bioinformatic analyses of clinical datasets. High GSDME expression associates with aggressive molecular subtypes, resistance to standard of care therapies, and diminished overall survival, suggesting its potential utility as a prognostic biomarker. This clinical linkage provides a compelling rationale for the development of GSDME-targeted diagnostics and therapeutics.
Notably, the research team also explored experimental approaches to reverse pyroptosis resistance by manipulating GSDME cleavage independently of endogenous regulatory hurdles. While pharmacologic or genetic activation of caspase-3 cleavage sites restored some pyroptotic sensitivity, glioblastoma cells compensated by invoking alternative survival pathways, underscoring the robustness of tumor adaptive mechanisms. These findings advocate for combinatorial strategies that simultaneously dismantle compensatory circuits alongside pyroptosis induction.
Insights from this investigation force a reevaluation of gasdermins as universal death effectors and call for nuanced frameworks appreciating their multifaceted roles in tumor biology. For glioblastoma, the dual identity of GSDME as both a potential tumor suppressor and a promoter of tumor progression exemplifies the complexity of programmed cell death regulation within malignancies with high adaptability and plasticity.
The implications of this work extend beyond glioblastoma. Other cancers with low pyroptotic responsiveness may similarly exploit gasdermin family member functions for survival and progression, highlighting a broader biological principle. Future research will need to dissect these context-specific roles and develop therapeutics capable of modulating gasdermin activity with precision, either restoring their death effector functions or mitigating their tumor-supportive roles.
In conclusion, Solel and colleagues have illuminated a counterintuitive yet mechanistically coherent paradigm wherein Gasdermin E, a protein classically associated with inflammatory cell death, imparts survival advantages and pro-tumoral functionalities in glioblastoma. This dualistic behavior reframes therapeutic targeting strategies, advocating for a more intricate understanding of programmed cell death machinery in glioblastoma and possibly other refractory cancers. As the field advances, harnessing or inhibiting GSDME’s multifaceted roles may become a cornerstone in developing next-generation glioblastoma therapies aiming to overcome the formidable barriers posed by this devastating disease.
Subject of Research:
Gasdermin E’s role in glioblastoma, focusing on pyroptosis resistance and tumor-promoting functions.
Article Title:
Gasdermin E in glioblastoma – pyroptosis resistance and tumor-promoting functions.
Article References:
Solel, E., Brudvik, E., Ystaas, L.A.R. et al. Gasdermin E in glioblastoma – pyroptosis resistance and tumor-promoting functions. Cell Death Discov. 11, 284 (2025). https://doi.org/10.1038/s41420-025-02572-z
Image Credits:
AI Generated
DOI:
https://doi.org/10.1038/s41420-025-02572-z
Tags: adaptive resistance mechanisms in glioblastomacaspase-3 activation in pyroptosiscell death modalities in cancer therapyGasdermin E in glioblastomaglioblastoma survival ratesglioblastoma tumor progression mechanismsimmunosuppressive microenvironment in brain tumorsinflammatory cell lysis in cancerprogrammed cell death pathways in cancerpyroptosis resistance in brain cancertherapeutic interventions for glioblastomatumor heterogeneity in glioblastoma
What's Your Reaction?