Border-Zone Cells Drive Heart Repair Protrusions
In the relentless pursuit to understand the mechanisms behind cardiac regeneration, a groundbreaking study has emerged, shedding light on the complex interplay between border-zone cardiomyocytes and macrophages in orchestrating extracellular matrix (ECM) remodeling. This intricate crosstalk is pivotal in promoting cardiomyocyte protrusion, a critical step in heart tissue regeneration, which has long eluded comprehensive mechanistic […]


In the relentless pursuit to understand the mechanisms behind cardiac regeneration, a groundbreaking study has emerged, shedding light on the complex interplay between border-zone cardiomyocytes and macrophages in orchestrating extracellular matrix (ECM) remodeling. This intricate crosstalk is pivotal in promoting cardiomyocyte protrusion, a critical step in heart tissue regeneration, which has long eluded comprehensive mechanistic understanding. The study, authored by Constanty, Wu, Wei, and colleagues, published in Nature Communications, represents a paradigm shift in how we perceive cellular coordination during cardiac repair, opening new avenues for therapeutic interventions in heart disease.
Cardiac regeneration has been a major focus in regenerative medicine because the adult mammalian heart notoriously exhibits limited regenerative capacity after injury, such as myocardial infarction. Traditional views have mostly centered on the intrinsic capacity of cardiomyocytes or stem cell-based strategies. However, this research distinctly highlights the nuanced role of the border zone—the area surrounding the infarct—where cardiomyocytes remain viable but are subjected to microenvironmental stressors and immune cell infiltration. The interplay in this niche appears to orchestrate a molecular and cellular symphony, whereby cardiomyocytes and immune cells collaboratively remodel the ECM, facilitating effective tissue regeneration.
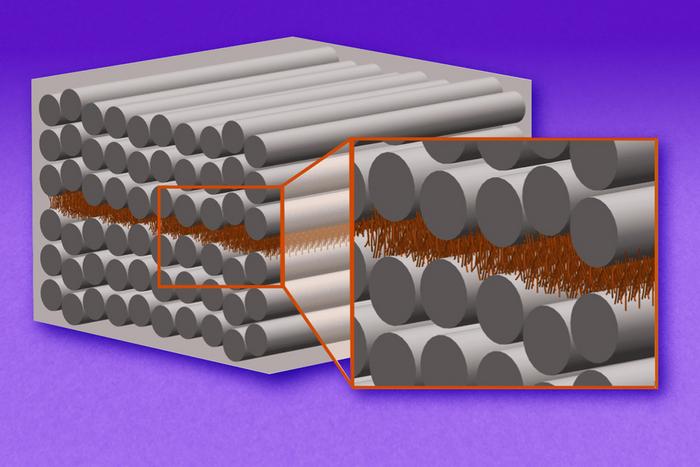
The extracellular matrix is far more than just a scaffold; it is a dynamic and highly regulated milieu that governs cell behavior, mechanical properties, and biochemical signaling. During cardiac injury, the ECM undergoes drastic changes, which if unbalanced, lead to fibrosis and adverse remodeling, impeding heart function. What Constanty et al. reveal is that macrophages infiltrating the border zone do not merely act as inflammatory responders but actively mediate ECM composition by secreting matrix metalloproteinases and cytokines that fine-tune the local environment. This remodeling, in turn, promotes the extension of cellular protrusions from border-zone cardiomyocytes, a phenomenon indicative of heightened cellular motility and possibly dedifferentiation or re-entry into the cell cycle.
Through the utilization of cutting-edge imaging techniques and molecular profiling, the study meticulously documents how cardiomyocyte protrusions physically interact with the remodeled ECM matrix. These protrusions appear to be essential mediators enabling cells to migrate and communicate over short distances, suggesting a coordinated effort in repopulating the damaged heart tissue. Supplementing these insights, transcriptomic analyses highlight the upregulation of integrins and cytoskeletal regulators in border-zone cardiomyocytes, which are known to be critical for protrusive activity and mechanotransduction.
One of the more fascinating aspects uncovered is the bidirectional signaling between macrophages and cardiomyocytes. Macrophages in the border zone shift toward a reparative phenotype, characterized by anti-inflammatory and pro-regenerative secretomes, which significantly influence the behavior of the cardiomyocytes. Conversely, cardiomyocytes emit signals that modulate macrophage function, fostering an environment conducive to healing rather than chronic inflammation. This dynamic feedback loop underscores the complexity and sophistication of innate immune interactions in tissue repair beyond their conventional roles.
The implications of these findings extend beyond basic biology; they offer a blueprint for therapeutic strategies aimed at harnessing or replicating this natural regenerative capacity. By targeting the signaling pathways and molecular mediators involved in ECM remodeling and cell protrusion, novel biomaterials or small molecule drugs could be designed to enhance cardiac repair post-infarction. For instance, modulating macrophage polarization or augmenting cardiomyocyte protrusion-promoting factors might mitigate scar formation and restore functional myocardium more effectively.
Moreover, this study challenges the existing dogma that cardiomyocytes in mammals are terminally differentiated and incapable of meaningful proliferation post-injury. The data suggest that, at least in the border zone, cardiomyocytes retain a latent plasticity, manifested through their ability to extend protrusions and potentially migrate or divide. This opens a compelling narrative that the microenvironmental context, particularly the ECM and immune cell landscape, significantly governs cardiomyocyte regenerative potential.
The detailed mechanistic insights gathered were made possible by innovative experimental models, including lineage tracing, in vivo imaging, and multiplexed immunostaining, which allowed the authors to visualize dynamic cellular behaviors in real-time within an intact myocardial setting. These technological advances are rapidly transforming regenerative research by enabling the dissection of complex spatiotemporal cellular interactions that were previously inaccessible.
Furthermore, the study touches on the critical balance between ECM degradation and synthesis during regeneration. Excessive degradation leads to structural instability, while insufficient remodeling precipitates fibrosis. The precise temporal and spatial control achieved by macrophages ensures the ECM remains malleable without compromising tissue integrity, enabling cell protrusions to navigate and anchor appropriately. This balanced remodeling is likely regulated by a tightly coordinated network of proteases, inhibitors, and growth factors.
Notably, the authors also discuss potential evolutionary underpinnings of this regenerative mechanism. Certain lower vertebrates capable of robust heart regeneration possess similar cardiomyocyte-immune cell-ECM interactions, suggesting a conserved biological program that mammals have attenuated. Understanding how to reactivate or enhance these pathways in humans could revolutionize treatments for heart failure.
In addition to therapeutic considerations, this research provides a new framework to reevaluate past experimental data on cardiac repair. It suggests that interventional studies aiming solely at boosting cardiomyocyte proliferation without addressing ECM remodeling or immune cell dynamics might be insufficient or suboptimal. An integrative approach that considers the multifaceted microenvironmental factors is thus paramount.
The multidisciplinary nature of the research team, comprising experts in cardiology, immunology, molecular biology, and bioengineering, reflects the complexity of cardiac regeneration as a field. This convergence of disciplines was instrumental in unraveling how cellular behavior is dictated by diverse but interconnected pathways, offering a more holistic understanding of myocardial repair processes.
Looking forward, the findings prompt several exciting research questions: How can the macrophage-cardiomyocyte dialogue be precisely manipulated in vivo? Are there unique molecular markers that distinguish regenerative macrophages that could be targeted? What are the long-term outcomes of enhanced cardiomyocyte protrusion in terms of electrical coupling and contractile function? Addressing these will be crucial for translating these discoveries into clinical reality.
In conclusion, Constanty et al.’s work marks a transformative step in decoding the cellular choreography that enables cardiac regeneration. Their elucidation of how border-zone cardiomyocytes and macrophages synergistically remodel the ECM to facilitate cardiomyocyte protrusion not only enhances fundamental biological understanding but also ignites new hope for regenerative therapies in ischemic heart disease. As heart failure continues to be a leading cause of mortality worldwide, such innovative insights pave the way toward reparative strategies that could restore heart function and substantially improve patient outcomes.
Subject of Research: Cellular mechanisms of cardiac regeneration focusing on interactions between border-zone cardiomyocytes, macrophages, and extracellular matrix remodeling.
Article Title: Border-zone cardiomyocytes and macrophages regulate extracellular matrix remodeling to promote cardiomyocyte protrusion during cardiac regeneration.
Article References:
Constanty, F., Wu, B., Wei, KH. et al. Border-zone cardiomyocytes and macrophages regulate extracellular matrix remodeling to promote cardiomyocyte protrusion during cardiac regeneration. Nat Commun 16, 3823 (2025). https://doi.org/10.1038/s41467-025-59169-4
Image Credits: AI Generated
Tags: border-zone cardiomyocytes rolecardiac regeneration mechanismscardiomyocyte protrusion processescellular coordination in cardiac repaircrosstalk between immune cells and cardiomyocytesextracellular matrix remodelingheart tissue regeneration strategiesmacrophages in heart repairmicroenvironmental stressors in heart injurymyocardial infarction recoveryregenerative medicine advancementstherapeutic interventions for heart disease
What's Your Reaction?