Autophagy: A New Target in RAS Cancers
In recent years, the field of oncology has witnessed a surge of interest in the intricate relationship between autophagy and oncogenic RAS-driven cancers. The latest insights presented by Üffing, Attridge, and Tooze in their groundbreaking 2025 publication in Cell Research illuminate a promising avenue that challenges traditional therapeutic paradigms. Their investigation delves deeply into how […]


In recent years, the field of oncology has witnessed a surge of interest in the intricate relationship between autophagy and oncogenic RAS-driven cancers. The latest insights presented by Üffing, Attridge, and Tooze in their groundbreaking 2025 publication in Cell Research illuminate a promising avenue that challenges traditional therapeutic paradigms. Their investigation delves deeply into how cancer cells exploit autophagy—a catabolic process traditionally associated with cellular housekeeping and survival—to fuel growth and resist treatment. This editorial aims to park a spotlight on the nuances of this alternative route to combat one of the most formidable oncogenic drivers in human malignancies: the mutated RAS protein family.
RAS mutations, particularly in KRAS, NRAS, and HRAS, represent some of the most frequently encountered oncogenic alterations in human cancers, including pancreatic, colorectal, and lung adenocarcinomas. These mutations play a critical role in driving cellular proliferation and survival, largely through dysregulation of intracellular signaling cascades such as the MAPK and PI3K pathways. However, direct pharmacological targeting of mutant RAS proteins has historically met with limited success due to their high affinity for GTP and lack of suitable binding pockets, rendering RAS “undruggable” for decades. Consequently, alternative strategies aiming to exploit downstream signaling intermediates or synthetic lethal partners have attracted considerable attention.
Üffing and colleagues zero in on one such alternative: autophagy. Autophagy, or “self-eating,” is a conserved lysosomal degradation pathway that recycles cellular components to maintain metabolic homeostasis. While autophagy is generally a survival mechanism under nutrient deprivation or stress, its role in cancer is paradoxical and context-dependent. In some settings, autophagy suppresses tumor initiation by limiting genome instability and chronic inflammation. Conversely, many established tumors, and especially those driven by RAS mutations, upregulate autophagy to meet elevated metabolic demands and survive in unfavorable microenvironments.
The authors meticulously dissect the complex interplay between RAS signaling and autophagic machinery. Oncogenic RAS fosters a rewiring of cellular metabolism that enhances nutrient scavenging, including reliance on autophagy-mediated degradation of intracellular constituents to sustain bioenergetic and biosynthetic processes. This metabolic rewiring enables cancer cells to thrive under hypoxic or nutrient-poor conditions, such as those imposed by a rapidly expanding tumor mass. Therefore, the study advances a compelling hypothesis that inhibiting autophagy could effectively ‘starve’ RAS-mutant tumors by cutting off a vital alternative supply line.
From a mechanistic standpoint, the study explores key nodes in the autophagy pathway that intersect with RAS-driven oncogenic signaling. For instance, downstream effectors of RAS, including mTOR and ERK, regulate autophagy initiation and flux, creating a finely tuned balance between growth promotion and catabolic recycling. Furthermore, RAS influences the expression of autophagy-related genes (ATGs), thereby enhancing the assembly and function of autophagosomes and lysosomes. Disruption of these pathways through genetic knockdown or pharmacological inhibition in experimental models led to marked reductions in tumor cell viability, underscoring the vulnerability imposed by autophagy dependence.
Intriguingly, the research highlights the dual impact of autophagy inhibition in RAS-mutant cells—not only does it impair metabolic flexibility, but it also potentiates DNA damage and endoplasmic reticulum stress, culminating in apoptotic cell death. This multifaceted susceptibility underscores why targeting autophagy may provide a synergistic benefit when combined with existing treatments such as chemotherapy or targeted inhibitors against RAS effectors.
Moreover, the study provides critical insights into tumor heterogeneity with respect to autophagy dependence. While many RAS-driven cancers appear to be “addicted” to autophagy, some subsets display compensatory metabolic adaptations that confer resistance to autophagy blockade. Unraveling these resistance mechanisms remains a pivotal challenge for therapeutic translation. The authors suggest that precision medicine approaches incorporating biomarkers of autophagic flux and metabolic profiling could stratify patients more likely to respond to autophagy inhibitors.
From a drug development perspective, several candidate molecules targeting autophagy-related processes are in various stages of clinical evaluation. Hydroxychloroquine, a lysosomal inhibitor used traditionally as an antimalarial, has shown modest efficacy in combination therapies, but lacks specificity. The quest for more selective inhibitors targeting upstream regulators such as ULK1, VPS34, or the ATG conjugation systems is rapidly evolving, inspired in part by findings such as those presented in this seminal work.
Importantly, the authors caution that systemic inhibition of autophagy may incur toxicities due to its essential roles in normal tissue homeostasis, especially in long-lived cells like neurons and cardiomyocytes. Therefore, advancing autophagy-targeted approaches will require ingenious delivery systems or pharmacodynamic strategies that preferentially affect tumor cells over normal tissues. Nanoparticle-mediated drug delivery, tumor microenvironment-responsive prodrugs, and intermittent dosing schedules are possible avenues to mitigate off-target effects.
The work also sheds light on the broader implications for cancer metabolism and therapeutic resistance. By illuminating autophagy as a metabolic lifeline in RAS-driven tumors, the study encourages a reevaluation of metabolic plasticity in cancer progression. It further suggests that a comprehensive anti-cancer strategy may necessitate simultaneous targeting of primary oncogenic drivers and the adaptive survival pathways they engage.
From a translational research angle, the study propels the incorporation of autophagy assays into early-phase clinical trials as pharmacodynamic readouts. This could facilitate real-time assessment of target engagement and optimization of combinatory regimens, including immunotherapies, where autophagy modulation might augment antigen presentation and immune cell infiltration.
Finally, this pioneering research by Üffing, Attridge, and Tooze positions autophagy not merely as a side character in the oncogenic narrative but as a central player and exploitable weakness in RAS-driven malignancies. Their findings beckon the scientific community to reframe existing dogma and embrace autophagy inhibition as a strategic front in the battle against cancers that have long evaded effective RAS-targeted therapies. As research progresses, this could herald a new chapter in oncology therapeutics, where the metabolism and recycling machinery of cancer cells become their Achilles’ heel.
Subject of Research: Autophagy mechanisms in RAS-driven cancers and their therapeutic targeting
Article Title: Targeting an alternative route: autophagy in RAS-driven cancers
Article References:
Üffing, A., Attridge, E. & Tooze, S.A. Targeting an alternative route: autophagy in RAS-driven cancers. Cell Res (2025). https://doi.org/10.1038/s41422-025-01127-2
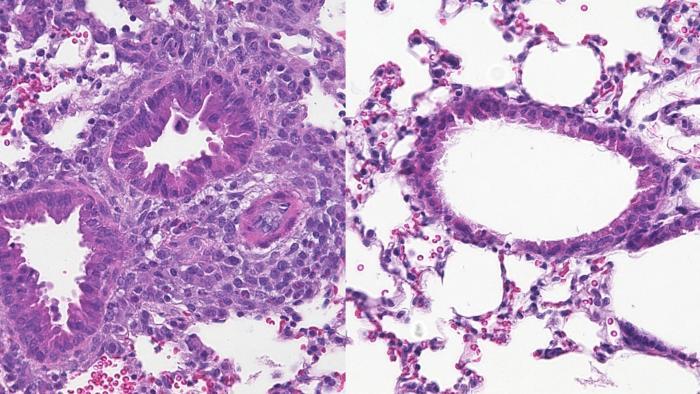
Image Credits: AI Generated
Tags: alternative cancer treatment strategiesautophagy and tumor growthautophagy in cancer therapybreakthroughs in cancer research 2025catabolic processes in cancer cellscellular survival mechanisms in cancerKRAS mutation and treatmentMAPK and PI3K pathways in oncologynovel approaches in oncologyoncogenic RAS-driven cancersresistance to cancer treatmenttargeting mutated RAS proteins
What's Your Reaction?