USC study reveals role of iron in allergic asthma and points to potential new therapies
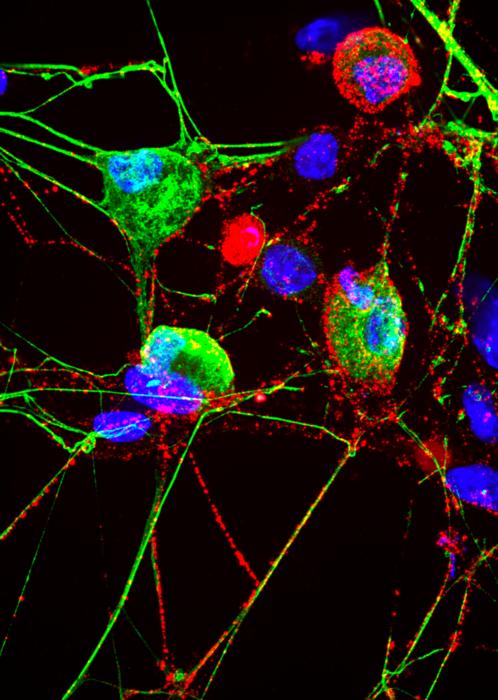
New USC research shows that iron serves as a gas pedal driving certain immune cells that cause inflammation in the lungs during an allergic asthma attack – and blocking or limiting iron may reduce the severity of symptoms. Credit: 2024 Hurrell et al. New USC research shows that iron serves as a gas pedal driving […]
New USC research shows that iron serves as a gas pedal driving certain immune cells that cause inflammation in the lungs during an allergic asthma attack – and blocking or limiting iron may reduce the severity of symptoms.
Credit: 2024 Hurrell et al.
New USC research shows that iron serves as a gas pedal driving certain immune cells that cause inflammation in the lungs during an allergic asthma attack – and blocking or limiting iron may reduce the severity of symptoms.
During an attack, immune cells known as group 2 innate lymphoid cells (ILC2s) can become overactive, causing excessive inflammation and a tightening of the airways, making it difficult to breath. However, the underlying biology is poorly understood.
Now, researchers from the Keck School of Medicine of USC have discovered key details about the mechanism behind the link, including that ILC2s depend on iron to generate energy. The findings could lead to new treatments offering relief to patients with asthma and a range of other allergic diseases.
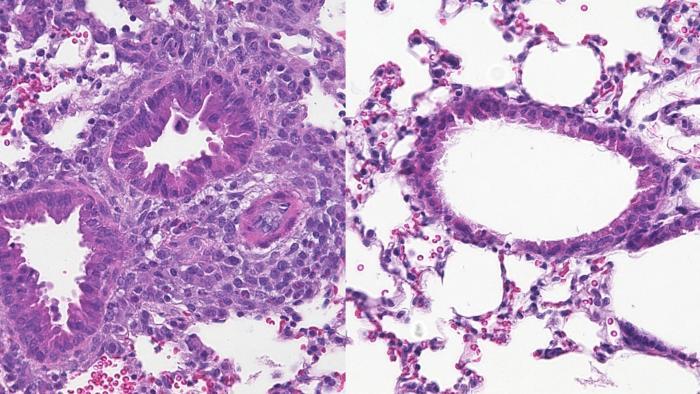
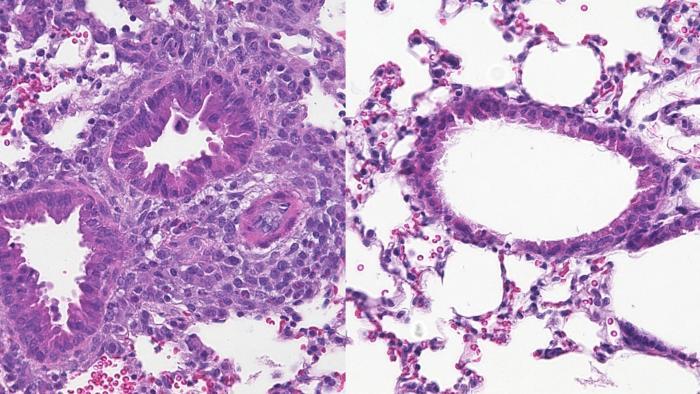
With support from the National Institutes of Health, the research team conducted a series of tests using both human cells and mouse models. They found that ILC2s use iron to fuel a range of cellular processes, therefore making it instrumental in activating the immune cells. In mice, preventing iron uptake in ILC2s reduced the severity of asthma symptoms. In human cells, increased ILC2 activity and iron uptake were correlated with asthma severity, suggesting that ILC2s and iron play an important role in more serious cases of the disease. The study was just published in the journal Science Translational Medicine.
“This is the first time it’s been shown that iron is an important metabolic regulator of pulmonary immune cells such as ILC2s, allowing them to generate energy. That’s helpful for treating disease, because targeting a cell’s energy can allow us to selectively increase or decrease its function,” said Benjamin Hurrell, PhD, a research assistant professor of molecular microbiology and immunology at the Keck School of Medicine and lead author of the study.
The findings build on the team’s broader research on ILC2s, including recent insights about a protein that may prevent the immune cells from becoming overactive in a study published in the Journal of Experimental Medicine. The researchers worked closely with the Keck School’s department of medicine, testing their findings in human cells to ensure they can move from the lab to the clinic as quickly as possible.
“We have limited drugs besides steroids for patients with asthma,” said Omid Akbari, PhD, a professor of molecular microbiology and immunology at the Keck School of Medicine and the study’s senior author. “Steroids inhalers and pills can control symptoms to keep patients alive, but they are not attacking the underlying pathophysiology of the disease. We hope our research can ultimately offer a better solution.”
The role of iron in asthma
To understand the role of iron in allergic asthma, the researchers first conducted a series of mechanistic studies, which are scientific investigations of the fundamental molecules, pathways and genes that underlie various biological processes.
In the body, iron enters cells by binding to a protein called transferrin. The researchers used a traceable form of transferrin, then activated ILC2 cells with an allergen. They observed transferrin entering the cells, proving that iron was also being taken up. When the researchers blocked ILC2 cells from absorbing transferrin (and iron), ILC2 activity dropped.
Blocking transferrin receptors is one way to prevent iron uptake in cells, but the researchers also tested their theory using another method: a substance called a chelator, that can bind to iron and restrict its availability for cells. The team used deferiprone, an iron chelator used to treat patients with a condition known as hemochromatosis, or iron overload. When they added deferiprone to cultured ILC2s, the result was the same: Iron availability decreased and so did ILC2 activity.
Next, the research team used single-cell RNA sequencing to analyze the transcriptomes of ILC2 cells. That analysis revealed that iron is a key part of the pathway for energy production in ILC2 cells.
In addition to mechanistic studies, the researchers tested the effect of limiting cellular iron availability in mouse models. Mice who received an iron chelator had less lung inflammation and airway hyperactivity—key features of asthma—compared to mice in a control group. In the absence of iron, ILC2s must adapt and generate energy in other ways, Hurrell said, which are associated with lower inflammation.
Finally, the team used cells from 36 patients with different asthma severities to further confirm that their findings will be useful for patients. They again showed that blocking iron uptake reduced the activation of ILC2 cells. They also found that cells from some donors had higher expression of a transferrin receptor, causing ILC2s to absorb more iron. That feature was correlated with more severe asthma, confirming a direct link between iron uptake and asthma in humans.
Targeting ILC2 cells
The results point to a new potential therapy for allergic asthma that, unlike steroid treatments, actually addresses the disease’s underlying cause.
“We can’t deplete a biological system of iron, which is an essential element for transporting oxygen in the body,” Akbari said. “But restricting iron availability to immune cells in the lungs could reduce the exacerbation of asthma during an acute attack. This approach also paves the way for treating other lung immune-mediated and inflammatory diseases, such as COVID-19.”
In addition, the findings could help provide relief for other allergic diseases, including eczema, dermatitis, hay fever, rhinitis and food allergies, in which ILC2 cells also become hyperactive.
Next, the researchers aim to find a restricted way to target ILC2 cells in the lungs, in order to reduce iron uptake locally without impacting other systems in the body.
About this research
In addition to Hurrell and Akbari, the study’s other authors are Yoshihiro Sakano, Stephen Shen, Doumet Georges Helou, Pedram Shafiei-Jahani, Mohammad Hossein Kazemi, Kei Sakano, Xin Li and Christine Quach from the Department of Molecular Microbiology and Immunology, Keck School of Medicine of USC; Richard Barbers from the Department of Medicine, Keck School of Medicine of USC; and Meng Li from the USC Libraries Bioinformatics Service, University of Southern California.
This work was supported by National Institutes of Health [R01 HL144790, R01 HL151493, R01 AI145813 and R01 HL159804].
Journal
Science Translational Medicine
DOI
10.1126/scitranslmed.adk4728
Method of Research
Experimental study
Subject of Research
Cells
Article Title
Iron controls the development of airway hyperreactivity by regulating ILC2 metabolism and effector function
Article Publication Date
8-May-2024
What's Your Reaction?