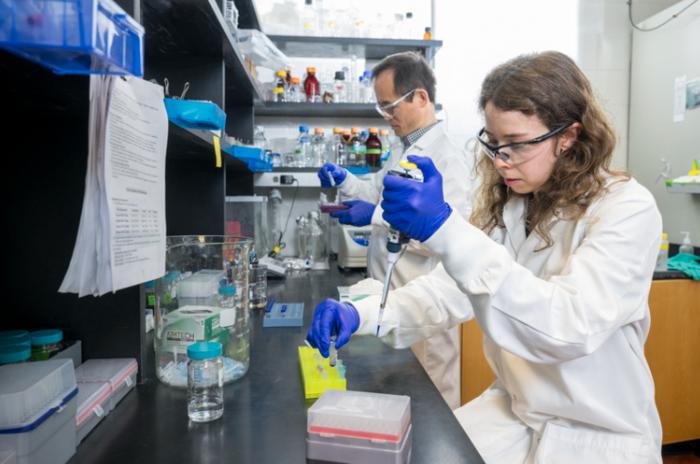
WVU scientists taking a close look at what causes immune cells to attack the central nervous system
A West Virginia University immunologist is exploring how the interaction between two types of immune cells within the central nervous system covering causes multiple sclerosis to develop. The findings could provide a pathway to new strategies for treating the disease and other neurological disorders. Credit: WVU Illustration/Aira Burkhart A West Virginia University immunologist is exploring […]

A West Virginia University immunologist is exploring how the interaction between two types of immune cells within the central nervous system covering causes multiple sclerosis to develop. The findings could provide a pathway to new strategies for treating the disease and other neurological disorders.

Credit: WVU Illustration/Aira Burkhart
A West Virginia University immunologist is exploring how the interaction between two types of immune cells within the central nervous system covering causes multiple sclerosis to develop. The findings could provide a pathway to new strategies for treating the disease and other neurological disorders.
Currently, about 2.3 million people worldwide are diagnosed with MS, an autoimmune disease that affects the central nervous system including the brain, spinal cord and optic nerves. It occurs when the immune cells that normally protect against viruses and bacteria instead attack the body. The initial immune activity takes place in the meninges, the three layers of membrane covering the brain and spinal cord that protects them from pathogens.
“We want to study how two immune cell types, T cells and monocytes, interact within the meninges before these immune cells go into the brain and the spinal cord and cause damage,” said Edwin Wan, associate professor in the WVU School of Medicine Department of Microbiology, Immunology and Cell Biology.
“We know that the interaction between T cells and monocytes in the meninges is critical for MS initiation, and potentially for the disease to progress as well. If we can identify the proteins that regulate the interaction of T cells and monocytes and how they respond and produce other factors to affect disease outcomes, these proteins can be targets for treating the disease.”
While there is no cure for MS, medications and therapeutic strategies aim to reduce the frequency of relapses. Currently, there is no effective medication to prevent disease progression.
The study is supported by a $2.5 million grant from the National Institute of Allergy and Infectious Diseases.
Wan and colleague Neil Billington, service assistant professor in the School of Medicine Department of Biochemistry and Molecular Medicine, and director of the Microscope Imaging Facility, will conduct the five-year project. Also assisting is Dr. Wen Zheng, a research scientist in the School of Medicine Department of Microbiology, Immunology and Cell Biology, and Kody Moore, of Fairmont, a student in the Immunology and Medical Microbiology undergraduate program.
For the study, researchers will use genetically modified mice and develop a live-imaging approach to monitor immune cell interactions in the spinal cord after induction of experimental autoimmune encephalomyelitis, a disease model in mice that mirrors MS in humans. With advanced imaging techniques they can view a time lapse of how the immune cells interact within a small area of the spinal cord where the activity is most intense.
“This is an especially innovative aspect of the project to study T cells and monocyte interactions in a live animal,” Wan said. “Using this technique, we can figure out the dynamic of the interaction and the outcome.”
Wan said he hopes learning more about the interactions between the central nervous system and the immune system can be applied to treating other neurological diseases.
“There is more and more recognition about the immune system’s involvement in neurological diseases such as Alzheimer’s disease and Parkinson’s disease,” he said. “In addition, we know that the immune system is also heavily involved in brain damage and recovery after stroke events, and both T cells and monocytes also play a role in that. I’m very interested to compare different responses of these immune cells toward different neurological diseases.”
Editor’s note: The use of animals in this project was evaluated by the WVU Institutional Animal Care and Use Ethics Committee. WVU is voluntarily accredited by AAALAC, a national peer organization that establishes a global benchmark for animal well-being in science.
What's Your Reaction?