Tumor deposits in colorectal and gastric cancers
This study is led by Prof. Yongzhan Nie (State Key Laboratory of Holistic Integrative Management of Gastrointestinal Cancers and National Clinical Research Center for Digestive Diseases, Xijing Hospital of Digestive Diseases, Fourth Military Medical University). Credit: ©Science China Press This study is led by Prof. Yongzhan Nie (State Key Laboratory of Holistic Integrative Management of […]
This study is led by Prof. Yongzhan Nie (State Key Laboratory of Holistic Integrative Management of Gastrointestinal Cancers and National Clinical Research Center for Digestive Diseases, Xijing Hospital of Digestive Diseases, Fourth Military Medical University).
Credit: ©Science China Press
This study is led by Prof. Yongzhan Nie (State Key Laboratory of Holistic Integrative Management of Gastrointestinal Cancers and National Clinical Research Center for Digestive Diseases, Xijing Hospital of Digestive Diseases, Fourth Military Medical University).
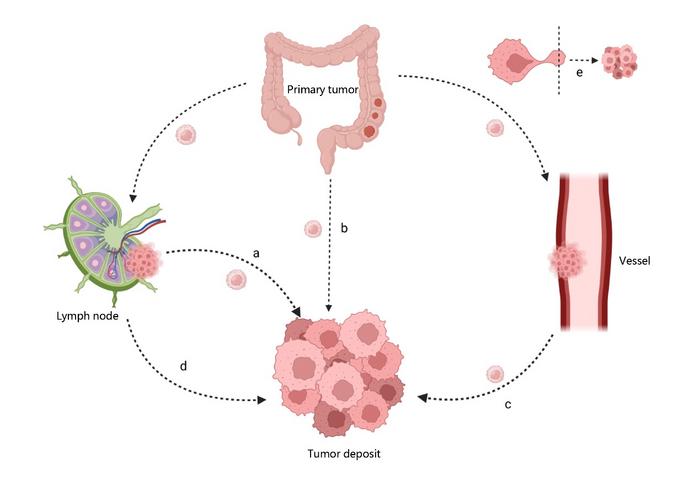
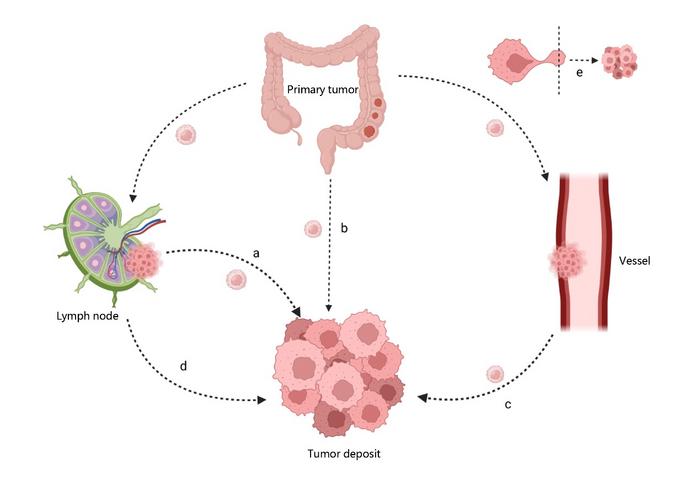
Tumor deposits (TDs), initially recognized in colorectal cancer, have been identified in various other cancer types, including gastric cancer. It is defined as aggregates of tumor cells found in adipose and fibrous tissues in the lymph node drainage area of a primary tumor. These deposits lack identifiable lymphoid structures and are not directly connected to the primary tumor. It is different from omental metastasis, TDs are regarded as local invasions of tumors in the range of gastric lymph node drainage, whereas omental metastasis is classified as distant metastasis. The 8th edition of TNM staging adopts stricter standards, defining TDs as tumor cell deposits without identifiable vascular or neural structures in addition to the absence of lymphatic structures. In sections stained with hematoxylin-eosin (H&E) or other staining methods, when a vessel wall or a neural structure is identified, it should be regarded as vascular invasion or perineural invasion, respectively. There is currently controversy over the structure and origin of TDs, and studies suggest that TDs are extracellular extensions of LNM or LNs replaced by tumor cells, resulting from either continuous growth or seeding from the primary tumor. The following figure shows several possible pathways of its formation.
Preoperative detection of TDs helps to elucidate their role and importance in tumor regression, thereby determining baseline tumor risk and determining the optimal preoperative treatment plan. However, the identification of TDs mainly relies on postoperative pathological diagnosis, lacking preoperative and intraoperative differentiation methods, which is not conducive to the early evaluation of tumors. The development of new imaging technologies and artificial intelligence has brought new possibilities for the preoperative identification of TDs.
TDs have been shown to significantly reduce the survival of patients with various types of tumors and are often associated with other unfavorable pathological factors. Meanwhile, it has also been reported that TDs increase the risk of liver, lung, and peritoneal metastases, reflecting the strong trend of tumor spreading and the potential for distant metastasis. But at present, the diagnosis of TDs mainly relies on postoperative pathological diagnosis, which is inconducive to the early evaluation of tumors, thus, it is beneficial for researchers to investigate preoperative imaging methods to predict TDs. However, those studies still have remarkable shortcomings, such as the small sample size and the lack of external test data.
TDs have been included in the TNM staging of colorectal cancer, which stipulated that regardless of the number, shape, and size of TDs, they were classified as signs of stage N1c disease if they did not present along with LNM. Changes in staging rules have led to an increase in the proportion of patients with stage Ⅲ and high-risk stage Ⅱ disease, indicating that an increasing number of patients need adjuvant therapy. However, TDs have not been involved in the TNM staging system for GC, related studies suggest that they can be incorporated in N or T staging, or labeled as high-risk factors. Irrespective of the modality by which TDs are incorporated into the T or N stage, the aim is to provide a more precise representation of the tumor’s characteristics at the histopathological level.
In conclusion, a consensus has been reached regarding the clinical significance and subsequent management of TDs. They have a detrimental impact on CRC and GC patients’ prognosis, emphasizing the necessity for thorough retrieval by surgeons and reporting on pathological reports by pathologists. Positive TDs indicate the need for more aggressive postoperative adjuvant therapy. However, controversies persist, and large-scale prospective studies are needed to explore the exact value of TDs in GC staging.
Journal
Medicine Plus
DOI
10.1016/j.medp.2024.100025
What's Your Reaction?

































