Study points to new approach to treat chronic transplant rejection
University of Pittsburgh researchers have identified a type of immune cell that drives chronic organ transplant failure in a mouse model of kidney transplantation and uncovered pathways that could be therapeutically targeted to improve patient outcomes. The findings are published in a new Science Immunology paper. Credit: UPMC University of Pittsburgh researchers have identified a type […]

University of Pittsburgh researchers have identified a type of immune cell that drives chronic organ transplant failure in a mouse model of kidney transplantation and uncovered pathways that could be therapeutically targeted to improve patient outcomes. The findings are published in a new Science Immunology paper.

Credit: UPMC
University of Pittsburgh researchers have identified a type of immune cell that drives chronic organ transplant failure in a mouse model of kidney transplantation and uncovered pathways that could be therapeutically targeted to improve patient outcomes. The findings are published in a new Science Immunology paper.
“In solid organ transplantation, such as kidney transplants, one-year outcomes are excellent because we have immunosuppressant drugs that manage the problem of acute rejection,” said co-senior author Fadi Lakkis, M.D., distinguished professor of surgery, professor of immunology and medicine, and scientific director of the Thomas E. Starzl Transplantation Institute at Pitt and UPMC. “But over time, these organs often start to fail because of a slower form of rejection called chronic rejection, and current medications don’t seem to help. Understanding this problem was the motivation behind our study.”
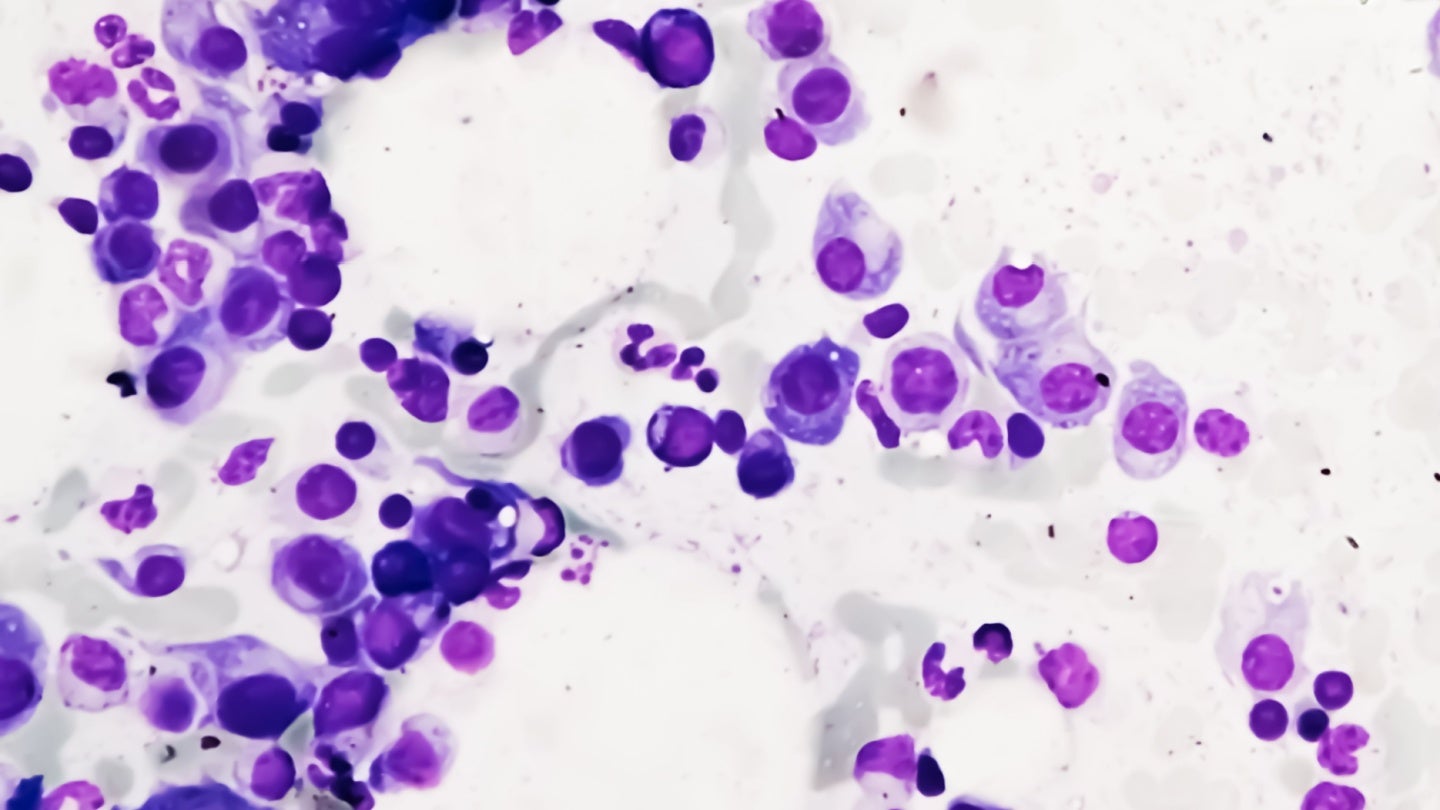
Previously, Lakkis and his colleagues had shown that a type of immune cell called tissue-resident memory T cells drive chronic rejection. Like all memory T cells, these resident versions “remember” previously encountered threats by recognizing specific identifying features called antigens. But unlike most memory T cells, which circulate in the bloodstream, tissue-resident memory T cells live within organs.
In the new study, first author Roger Tieu, Ph.D., Medical Scientist Training Program student at Pitt, discovered two factors that maintain resident memory T cells in kidney grafts over time. The first is the antigen itself — the molecules that T cells use to recognize the donor graft as foreign. Because resident T cells dwell within the kidney graft, they’re constantly exposed to such antigens. The second factor is a cytokine, or inflammatory signaling protein, called IL-15.
Also key to this process is another type of immune cell called dendritic cells, which capture both the antigen and IL-15 and present them to receptors on resident memory T cells.
“Dendritic cells are like the conductor of the orchestra,” said Lakkis. “They’re critical for activating many types of immune cells and coordinating immune responses.”
When the researchers depleted dendritic cells or blocked their ability to present antigen or IL-15, they saw a drop in resident memory T cell quantity and functionality.
“Antigen and IL-15 are required for T cell maintenance,” said co-senior author Martin Oberbarnscheidt, M.D., Ph.D., assistant professor of surgery at Pitt. “If you remove either, resident memory cells decline in number. In a transplant patient, it’s not feasible to take the antigen away because it’s found throughout the donor organ, but targeting IL-15 is clinically translatable.”
Indeed, when the researchers blocked IL-15 signaling with an antibody that prevented IL-15 binding to its receptor on T cells, they found that graft survival was greatly prolonged in mouse kidney recipients.
The researchers hope that the findings could set the stage for clinical trials to test the antibody in transplant patients to minimize chronic rejection. Blocking IL-15 signaling could enable more precise targeting of resident memory T cells within the graft, while minimizing global immunosuppression of other T cells throughout the body that are important for immunity to infections.
“In my medical school training, I have had the privilege of working with transplant patients,” said Tieu. “I am excited that our work has the potential to be translated from lab to clinic, with the goal of mitigating chronic rejection and elevating quality of life for our patients.”
Other authors on the study were Daqiang Zhao, M.D., Ph.D., Gang Zhang, M.D., Neda Feizi, Ph.D., Priyanka Manandhar, Amanda L. Williams, M.S., Benjamin Popp, M.S., Michelle A. Wood-Trageser, Ph.D., Anthony J. Demetris, M.D., Lawrence P. Kane, Ph.D., Khodor I. Abou-Daya, M.D., and Warren D. Shlomchik, M.D., of Pitt or UPMC; Qiang Zeng, M.D., Nationwide Children’s Hospital; J. Yun Tso, Ph.D., JN Biosciences; and Aaron J. Johnson, Ph.D., Mayo Clinic.
This research was supported by the National Institutes of Health (R01 AI049466, R01 AI145881, R01 HL143349, R01 GM136148, R01 NS103212, T32 GM008208, T32 AI074490, F30 DK124925, 1S10OD011925-01 and 1S10OD019942-01) and the American Society of Transplantation.
##
Journal
Science Immunology
DOI
10.1126/sciimmunol.add8454
Method of Research
Experimental study
Subject of Research
Animals
Article Title
Tissue-resident memory T cell maintenance during antigen persistence requires both cognate antigen and interleukin-15
Article Publication Date
21-Apr-2023
What's Your Reaction?