Sepsis: Unraveling the Fatal Consequences of a Silent Threat
Recent research conducted by a team at the UConn School of Medicine has unveiled a critical new understanding of the biological mechanisms at play during sepsis, one of the leading causes of death globally. Every year, sepsis claims approximately 11 million lives worldwide, as reported by the World Health Organization. This life-threatening condition is marked […]


Recent research conducted by a team at the UConn School of Medicine has unveiled a critical new understanding of the biological mechanisms at play during sepsis, one of the leading causes of death globally. Every year, sepsis claims approximately 11 million lives worldwide, as reported by the World Health Organization. This life-threatening condition is marked by severe inflammation in response to infection, which can lead to multiple organ failure, shock, and ultimately death. Intriguingly, this new research proposes that the inflammation is largely incited not by the infectious agent itself, but by the behavior of host cells navigating the crisis.
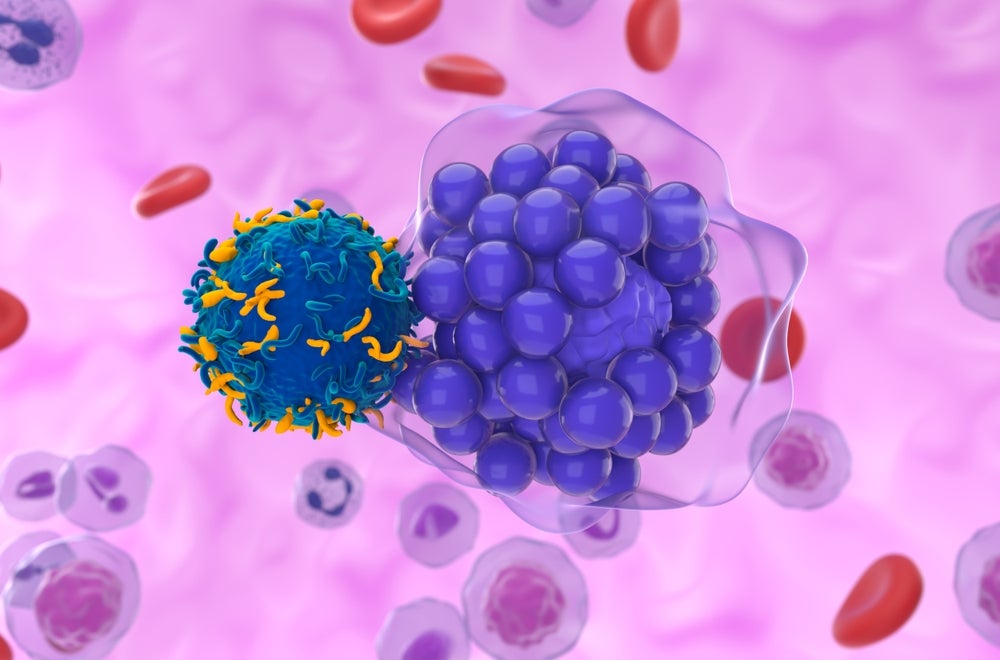
When infection occurs, some cells become infected and are compelled to self-destruct to prevent the spread of pathogens. This form of cell death, known as pyroptosis, is characterized by the release of pro-inflammatory signals and cell contents, thereby amplifying the inflammatory response. Rather than merely disposing of the threat, dying cells send out distress signals that can influence their neighboring cells. As these neighboring cells receive these signals, they mistakenly activate similar death pathways, perpetuating a cycle of cell death and inflammation. This discovery hints at a profound insight into how localized cell death might spiral out of control, leading to widespread systemic inflammation during sepsis.
The authors of the study suggest that understanding this “deadly messaging” could provide a pivotal opportunity for therapeutic intervention. When cells undergo pyroptosis, they allow the translocation of a protein known as gasdermin-D. This protein is integral to forming pores within the cell membrane, leading to the aforementioned leakage of cellular contents. Researchers have identified that when cells manage to eject these gasdermin-D containing membrane portions, they inadvertently produce extracellular vesicles. These vesicles carry the deadly gasdermin-D pore, establishing a conduit of destruction as they circulate and interface with surrounding healthy cells.
The team, led by immunologist Vijay Rathinam, notes that this unintentional messaging of death can lead to a rapid reduction in healthy cell populations in the area near the original infection. In this manner, researchers observed that a cluster of dying cells could release enough of these vesicles to turn a local inflammatory response into a catastrophic system overload. Essentially, the very act of individual cells trying to self-preserve can collectively catalyze a lethal cascade capable of overwhelming the immune system—an ironic twist of biology, underscoring how the cellular survival instinct can become a weapon of mass destruction.
As the research advances, the team is dedicated to exploring potential targets within this pathway that could be disrupted to halt the transmission of the lethal signal among cells. If successful, this could lead to innovative interventions for various inflammatory diseases, particularly sepsis. A clear understanding of the mechanism by which gasdermin-D propagates this cell death among bystander cells can help design drugs or therapies that interrupt this destructive communication channel.
Moreover, the findings contribute to a growing narrative in immunology, where the role of cellular communication in inflammation is increasingly recognized. This research paints a complex picture of how our immune system responds to stress and infection, presenting new perspectives on how inflammation, a typically protective response, can veer into harmful territory. The implications of such work reach far beyond sepsis and could reshape our understanding of other inflammatory and autoimmune conditions as well.
The collaboration among researchers at UConn School of Medicine exemplifies the interdisciplinary approach required to tackle such questions. By leveraging expertise in cell biology, immunology, and experimental methodologies, the research brings to light the multifaceted interactions involved in cellular stress responses. The hope is to translate these laboratory insights into clinical outcomes that can save lives by curbing avoidable cell death during inflammatory diseases.
While this study focuses on the nuances of gasdermin-mediated processes, broader questions regarding the role of other inflammatory mediators also emerge. For instance, how do various cells within the immune response communicate and regulate each other? What specific signals lead to changes in neighboring cell behavior? Future research may need to delve deeper, unraveling the intricate web of cellular interactions that governs various aspects of immune response, homeostasis, and pathology.
This study is just a step in the larger endeavor to comprehend and control sepsis and similar inflammatory ailments. The insights gleaned could prompt further investigation into targeted therapies that inhibit the detrimental effects of pyroptosis while preserving the necessary immune functions that protect against infection. An optimized balance is paramount; the challenge lies in clamping down on cell death driven by inflammation without compromising the body’s ability to fight infections effectively.
In summary, the research emerging from the UConn School of Medicine represents a significant advancement in understanding cell death, inflammation, and their role in catastrophic conditions like sepsis. There exists a delicate interplay between cellular mechanisms of self-preservation and the devastating effects these same mechanisms can have on neighboring cells, highlighting the complex nature of biological responses to infection. Through persistent research efforts aimed at tightening our grip on these processes, the day may soon come when we can mitigate the harsh outcomes of sepsis effectively.
Subject of Research: Cells
Article Title: Transplantation of gasdermin pores by extracellular vesicles propagates pyroptosis to bystander cells
News Publication Date: 23-Jan-2025
Web References: Cell Article
References: NIH/National Institutes of Health
Image Credits: N/A
Keywords: Sepsis, Cell membranes, Inflammation, Cellular processes, Inflammatory disorders, Cell pathology, Cell biology, Cell death, Cell behavior, Cell survival.
Tags: cell death and immune responseconsequences of sepsishost cell behavior in sepsisinflammatory response in infectionsmechanisms of severe inflammationorgan failure due to sepsispyroptosis and inflammationresearch on sepsis treatmentsepsis biological mechanismssepsis global mortality statisticssilent threats in healthcareunderstanding sepsis inflammation
What's Your Reaction?