Revolutionizing Treatment: Microbubble Precision Therapy Takes Center Stage
The challenge of treating brain diseases such as Alzheimer’s, Parkinson’s, and brain tumors is a complex task, primarily due to the brain’s unique architecture and the protective barrier it possesses. This so-called blood-brain barrier plays a crucial role in maintaining central nervous system homeostasis by selectively allowing certain molecules like nutrients and oxygen to pass […]


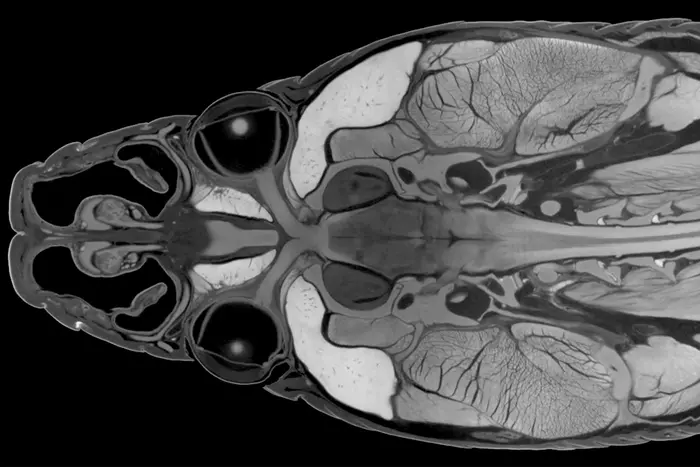
The challenge of treating brain diseases such as Alzheimer’s, Parkinson’s, and brain tumors is a complex task, primarily due to the brain’s unique architecture and the protective barrier it possesses. This so-called blood-brain barrier plays a crucial role in maintaining central nervous system homeostasis by selectively allowing certain molecules like nutrients and oxygen to pass through while blocking out potentially harmful substances, including a vast majority of therapeutic agents intended for brain diseases. Researchers have long sought effective methods to bypass this barrier, and recent advancements have opened promising pathways to deliver therapies directly to the brain, enhancing the possibility of successful treatments.
One of the most exciting methods moving to the forefront of this research involves the use of ultrasound-responsive microbubbles. These microbubbles present a novel delivery system, being significantly smaller than red blood cells and filled with gas, featuring a specialized lipid coating that provides stability and functionality. The concept is simple yet profound: microbubbles are injected into the bloodstream along with therapeutic drugs and can be activated using ultrasound at targeted sites. This sonic activation induces the microbubbles to oscillate rapidly, leading to the formation of minute pores in the endothelial cell membranes of blood vessels, through which the drugs can efficiently transit.
Understanding the mechanism by which ultrasound-activated microbubbles create these pores has remained a mystery until now. A research team from ETH Zurich, under the guidance of Professor Outi Supponen at the Institute of Fluid Dynamics, has made notable progress in elucidating this phenomenon. Their groundbreaking study, recently published in the journal Nature Physics, reveals that exposure to ultrasound causes the microbubble surfaces to distort, forming unique liquid jets, termed microjets, which effectively penetrate the endothelial cell membrane.
The research demonstrates that these microjets, propelled by immense force, reach velocities as high as 200 kilometers per hour, allowing them to deliver therapeutic agents with unmatched precision while preserving the integrity of the surrounding cells. This represents a remarkable advancement in biomedical engineering, particularly for the treatment of delicate and complex brain conditions. By forming targeted pinprick-like entries into the membranes, the microjets facilitate a highly localized method of drug delivery that minimizes collateral damage to surrounding tissue.
Studies leading up to this discovery faced substantial challenges, primarily due to the microscopic scale of the phenomena involved. Traditional observational methods utilizing standard microscopy typically only capture information from above, rendering the actual interaction between microbubbles and cells nearly invisible. To overcome these challenges, the research team engineered a specialized side-view microscope capable of 200x magnification, coupled with an advanced high-speed camera that captures up to ten million frames per second. This setup allowed for unprecedented insights into microbubble dynamics and their interactions with cellular structures.
Upon experimentation, the researchers constructed a model that mimicked the blood vessel wall by culturing endothelial cells on a plastic membrane. This membrane was subsequently immersed in a saline solution containing a model drug, allowing for the natural ascent of microbubbles to the cell layer. Administered via quick pulses of ultrasound, these microbubbles were made to vibrate, simulating conditions that would occur in a real physiological environment.
An intriguing finding of the study is the observation that at elevated ultrasound pressures, microbubbles no longer retain their spherical form but instead adopt complex, lobular shapes that rhythmically oscillate, pushing inwards and outwards. This cyclical movement is critical as it allows inward-folded lobes to sink deeper with each cycle, eventually leading to significant liquid ejection jets that extend far enough to permeate the cell membrane.
What’s particularly exciting is that this jetting mechanism operates effectively under relatively low ultrasound pressures—around 100 kilopascals—comparable to atmospheric pressure. This ensures that the procedure is not only feasible within a clinical setting but also reduces potential risks associated with high-pressure applications. The implications for patient safety are vast, especially considering that few ultrasound pulses are sufficient to achieve membrane perforation.
The researchers believe that their findings provide a concrete physical basis for refining drug delivery mechanisms using microbubbles and pinpoint the criteria necessary for their safe application. The critical parameters of ultrasound frequency, pressure, and microbubble dimensions can now be calibrated to optimize therapeutic outcomes while ensuring minimal risk to the patient. Furthermore, the study opens avenues for fine-tuning the microbubble surface properties to make them more responsive to specific ultrasound frequencies, ensuring efficient jet formation.
This research holds significant promise for the future of drug delivery systems, particularly in treating complex neurological disorders. By unveiling the intricacies of microbubble behavior and their interactions with cell membranes, the team has paved the way for novel therapeutic approaches that could transform the treatment landscape for diseases that have remained intractable for far too long. The pursuit of enhanced drug delivery methods via advanced physical dynamics epitomizes a significant stride towards merging physics and medicine for patient benefit.
As researchers continue to gather insights from their observations and theoretical modeling of microbubble interactions, they bring closer the realization of effective, non-invasive therapies that could change the lives of countless individuals suffering from brain diseases. Moreover, the platform established by their study serves as a springboard for investigating new microbubble formulations designed by other scientists, fostering greater collaboration in the field as they strive to solve some of medicine’s most challenging puzzles.
With further refinement and validation, microbubble-mediated drug delivery may soon become a standard practice in the treatment of neurological conditions. As science progresses, the integration of these innovative techniques into clinical applications will undoubtedly require rigorous testing and monitoring. Still, the findings herald a new dawn for therapeutic interventions, characterized by precision and safety that could herald significant improvements in patient outcomes in the years to come.
In summary, this research not only provides clarity on the operational mechanisms behind microbubble-mediated therapies but also signals a transformative era in drug delivery processes, emphasizing the invaluable role of interdisciplinary approaches in driving innovation in medicine.
Subject of Research: Microbubble-mediated drug delivery using ultrasound
Article Title: Unveiling the Mechanism of Microbubble-Mediated Drug Delivery Through Ultrasound
News Publication Date: October 2023
Web References:
References: Cattaneo M, Guerriero G, Gazendra S, Krattiger L, Paganella L, Narciso M, Supponen O, Cyclic jetting enables microbubble-mediated drug delivery, Nature Physics (2025), DOI: 10.1038/s41567-025-02785-0
Image Credits: Not provided.
Keywords
Microbubbles, Drug Delivery, Ultrasound, Blood-Brain Barrier, Alzheimer’s Disease, Parkinson’s Disease, Endothelial Cells, Therapeutic Agents, High-Speed Imaging, Medical Physics, Nanotechnology, Neuroscience.
Tags: Alzheimer’s treatment advancementsbrain tumor treatment innovationsenhancing CNS therapy effectivenessmicrobubble precision therapymicrobubble technology in medicinenon-invasive brain treatment strategiesnovel therapeutic methodsovercoming blood-brain barrierParkinson’s disease therapiestargeted drug delivery systemstreating brain diseasesultrasound-responsive drug delivery
What's Your Reaction?