Rejuvenating Aging Mice by Reactivating Senescent Cells
Imagine a world in which aging cells, once written off as irreversible markers of decline, suddenly rediscover how to divide and renew themselves, effectively pushing back the relentless march of time. That is precisely the breathtaking scenario emerging from a study on exosomal microRNA, specifically miR-302b, which has captured the attention of scientists by revealing […]


Imagine a world in which aging cells, once written off as irreversible markers of decline, suddenly rediscover how to divide and renew themselves, effectively pushing back the relentless march of time. That is precisely the breathtaking scenario emerging from a study on exosomal microRNA, specifically miR-302b, which has captured the attention of scientists by revealing a path to rejuvenation in aging mammalian tissues. Researchers publishing their work in an article entitled “Exosomal miR-302b rejuvenates aging mice by reversing the proliferative arrest of senescent cells” have ventured into the heart of what defines aging on a cellular level, uncovering an extraordinary intervention that may one day allow individuals to live longer, healthier, and more active lives. As we delve into the mesmerizing details of this discovery, we find ourselves confronted with the possibility of upending conventional assumptions about the finality of cellular senescence, an intriguing concept that offers a glimpse into the ever-shifting boundaries of biological knowledge.
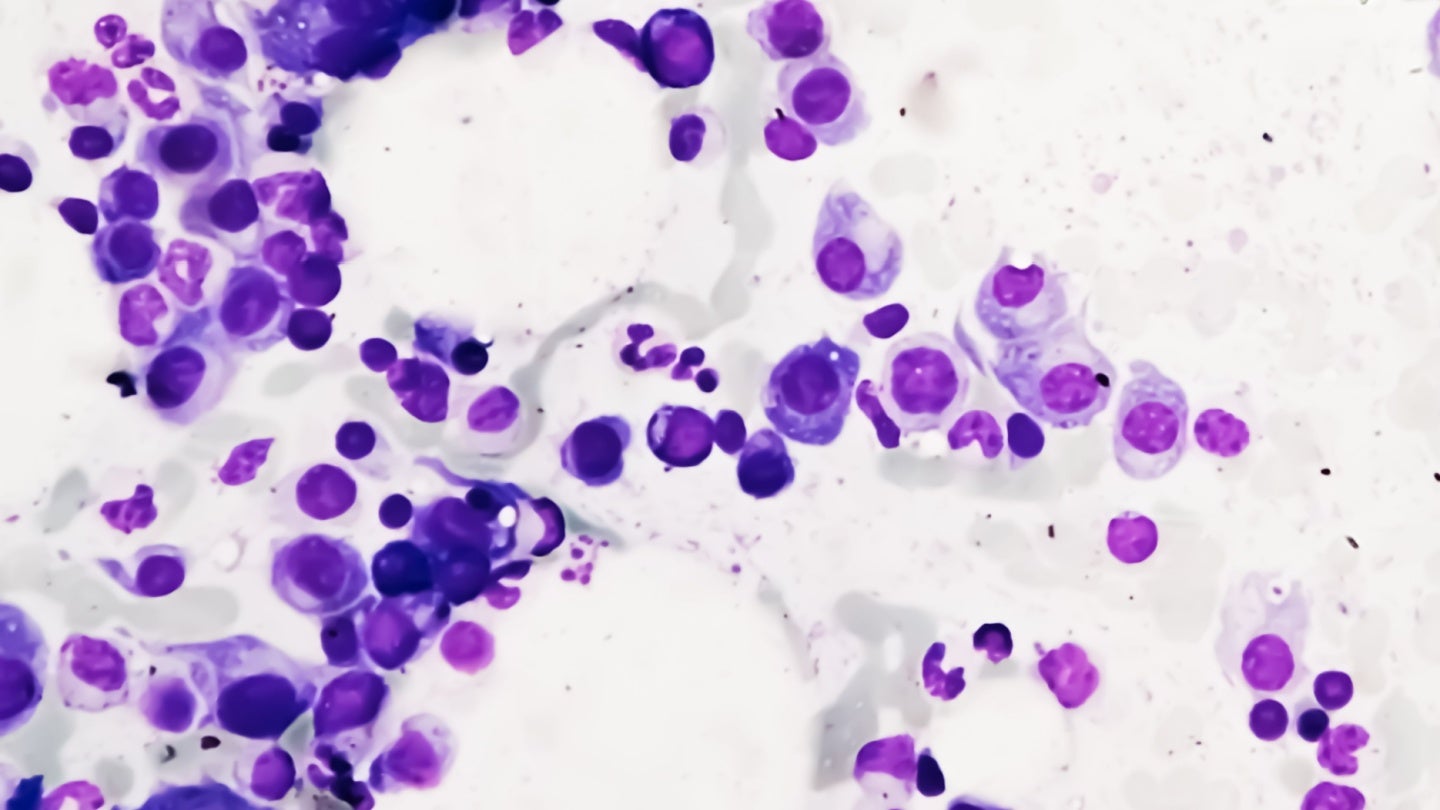
To appreciate this story, we first need to understand the significance of cellular senescence, a state in which cells exit the cell cycle and remain in a type of permanent arrest. Senescent cells, or SnCs as they are sometimes abbreviated, accumulate with age, building up across tissues and secreting a pro-inflammatory set of factors known as the senescence-associated secretory phenotype. The common wisdom in biology has been that cellular senescence serves as a protective stop sign for damaged or stressed cells, preventing them from turning cancerous. However, as these SnCs collect in older tissues, their presence sparks chronic inflammation, tissue dysfunction, and a range of detrimental effects associated with aging. The standard approaches to mitigate their impact often rely on purging them from the body (the senolytic method) or suppressing their inflammatory signals (the senomorphic method). Both strategies bring their own set of complications, prompting the pursuit of alternate solutions, ones that might rescue SnCs and coax them back into a functional state.
This is where exosomal miR-302b steps into the limelight. Exosomes are minuscule vesicles, typically 30 to 150 nanometers in diameter, that bud off from the membranes of cells. Human embryonic stem cell-derived exosomes, known in the study as hESC-Exos, contain a wealth of proteins, nucleic acids, and microRNAs, each capable of influencing fundamental processes like growth, repair, and inflammation. Among the most prevalent cargo items discovered in hESC-Exos was a particular microRNA named miR-302b. MicroRNAs can bind to specific messenger RNAs within cells, reducing their expression. In the case of miR-302b, it appears to target two major regulators of cell cycle arrest: Cdkn1a and Ccng2. By dampening these regulators, miR-302b seemingly releases senescent cells from their stagnant condition, restoring the proliferative capacity once thought to be irreversibly lost. The idea that we can restore old or stressed cells to a more youthful state, rather than simply killing them off, is as enthralling as it is unexpected.
During in vitro experiments, hESC-Exos were administered to senescent human fibroblast cells. These fibroblasts, known as IMR-90, had undergone the typical trajectory of aging, culminating in what is termed replicative senescence. After exposure to the purified exosomes for 72 hours, the cells displayed a marked decline in well-established senescence markers, such as SA-β-gal activity and high levels of p21 and p16. More strikingly, these rejuvenated cells began proliferating again, suggesting that the exosomes had reversed their once-stable proliferative arrest. To confirm that miR-302b was the key factor, tests were performed with direct miR-302b overexpression. This intervention was sufficient to reproduce the same anti-senescence effects, effectively exonerating other molecules in hESC-Exos from prime responsibility. It was in these momentous observations that the notion of “Senoreverse” took shape, pointing to a strategy that can do far more than moderate senescence; it can apparently make it yield to renewed vigor.
Beyond cell culture dishes, the study investigated what might happen if older mice were dosed regularly with hESC-Exos or with exosomes loaded explicitly with miR-302b. To begin with, the scientists wanted to confirm that such exosomes were not tumorigenic. After all, hESC-Exos originate from cells that are part of the embryonic blueprint, raising concerns about their capacity to unleash unfettered cell division. Reassuringly, mice that were injected systematically with these exosomes over multiple months failed to present heightened rates of tumors or other severe complications. This safety check paved the way for a longevity analysis to be undertaken with the exosome or miR-302b therapy. The results were dramatic: mice that received hESC-Exos displayed extended survival, with both the median and maximum lifespans surpassing those of their untreated peers. From a morphological standpoint, the animals on therapy appeared younger, exhibiting healthier fur, improved muscle strength, superior coordination, and reduced chronic inflammatory markers. At a cellular level, analysis of multiple tissues (kidney, liver, lung, spleen, and skin) showed diminished senescence signals, reduced expression of p21 and other senescence-related genes, plus an encouraging rise in cells in the S-phase of the cell cycle. The body’s tissue landscapes, typically beleaguered by the ravages of aging, took on a renewed vibrancy, hinting that the therapy did more than just remove a handful of problem cells. Rather, it coaxed them back to function.
Subsequent single-cell RNA-seq data underscored these findings. Senescent cells in the livers and skin of older mice treated with hESC-Exos or miR-302b underwent remarkable transcriptomic shifts, pushing them away from a senescent profile and toward an intermediate or rejuvenated one. Genes involved in the G1/S checkpoint, S-phase progression, or G2/M transition were upregulated, whereas those that force cells out of the cell cycle, like Cdkn1a and Ccng2, were suppressed. The repeated emphasis on these two checkpoint genes suggested they are not mere bystanders but central to controlling the onset and maintenance of senescence. It is as though the exogenous miR-302b floods the regulatory system and seizes these gatekeeper checkpoints, flinging the door wide open for a quiet cell to rejoin the dance of proliferation.
In a further step, the team used an advanced technique called Ago2 Clip-seq, capturing the RNAs bound to Argonaute 2, the main effector of microRNA-mediated silencing. This method validated that miR-302b directly interacts with the 3′ untranslated regions of Cdkn1a and Ccng2 transcripts, dampening their expression. Interestingly, a wide swath of other potential gene targets also surfaced in Clip-seq results. In general, these were skewed toward cell cycle reactivation, DNA repair, or anti-aging pathways, raising the possibility that miR-302b is orchestrating a broad pro-proliferation and pro-rejuvenation cascade. The four to five more intensively validated target genes, though, appear to be the fulcrum.
One might pause to ask: if older mice can spontaneously re-emerge with stronger muscle function, sharper cognition, and more robust tissues, might that not come at a cost, such as igniting rampant tumorigenesis or interfering with processes that keep cells in check? After all, the presence of senescent cells is typically portrayed as a cancer-suppressive mechanism, halting any runaway proliferation in cells harboring DNA damage or oncogenic mutations. The investigators specifically tested that concern by carefully analyzing any potential tumor burdens over the course of up to 24 months of repeated therapy. The result? No surge in tumors or disease burden emerged in animals receiving the exosomes or miR-302b. Indeed, the cause-of-death distribution was statistically indistinguishable from that in the untreated, aging controls. This outcome implies that the reactivation of older cells into proliferation can be carefully orchestrated without unleashing cancer, though extended or new contexts might still reveal complexities. Additional research is needed to verify these findings in diverse genetic backgrounds and in animals predisposed to certain cancers, ensuring that the approach is as safe as these initial results suggest.
Of course, a puzzle remains: how might reactivated cells in aging tissues maintain genomic integrity? Typically, a major impetus behind senescence is the presence of telomere attrition, DNA double-strand breaks, or other forms of genomic instability. When cells break free from senescence, they might risk replicating damaged DNA. Yet the current analysis discovered an uptick in H3K9me3, a marker associated with chromatin stability, and a reduction in γ-H2AX, an indicator of active DNA damage response, in older tissues treated with exosomes or miR-302b. The data raise the speculation that reactivated cells might also heighten their DNA repair pathways, possibly aided by factors inside the exosomes. Indeed, exosomes from hESCs are known to hold a variety of pro-regenerative molecules, so the synergy might well be broader than the single microRNA. Because the investigators singled out miR-302b as the prime agent, it is possible that its manipulation fosters a more stable re-entry to the cell cycle by synchronizing the reduction in DNA damage signals with the upregulation of replication competence.
Another intriguing angle is the interplay between reactivated SnCs and the immune system. Under normal conditions, senescent cells, through their SASP, help recruit immune cells to clear them away. Chronic inflammation arises if the immune system fails to keep pace, leaving SnCs to accumulate and degrade tissue function. If reactivated SnCs produce fewer inflammatory signals and reacquire a more youthful functional state, then we might imagine that SASP-driven persistent inflammation subsides, enabling tissues to run more smoothly, with less infiltration of immune elements. That is consistent with the observation of decreased inflammatory markers in the circulation of older mice receiving exosomal miR-302b. This scenario diverges from common senolytic or senomorphic treatments that either kill SnCs or muzzle the SASP, possibly interfering with beneficial immune surveillance. The newly proposed approach spares these cells from destruction, effectively staves off their inflammatory secretions by letting them rejoin the workforce of dividing cells, and so might neatly evade the pitfalls of other therapies.
Translating these results into any kind of future therapy for humans requires a great deal of caution and more specialized knowledge. The embryonic origin of hESC-Exos can spark ethical debates or safety concerns. The authors addressed tumorigenicity in mice, but the immunocompatibility or potential for immune responses in humans remain uncertain. Similarly, for large-scale production, repeated injections, and quality control, many standardization challenges loom. The direct usage of exosomes from embryonic stem cells might be further complicated by regulatory or ethical constraints. For these reasons, the scientists delved deeper, concluding that the essential factor was miR-302b, something that can be synthesized or carried by more easily standardized exosome carriers or even lipid nanoparticles. Indeed, in the latter part of the research, the authors used 293F cells to produce exosomes that were then loaded via electroporation with synthetic miR-302b. Administration of these prepared exosomes produced the same broad rejuvenation results as seen with hESC-Exos, culminating in older animals living longer, healthier lives. This shift into an off-the-shelf approach for delivering a single microRNA stands as a strong impetus for further investigations aimed at bridging preclinical success to clinical trials.
On a broader scale, we see the concept of “Senoreverse” emerging, with its powerful notion of reversing, rather than eliminating, senescent cells. This story resonates with the grand puzzle in aging research: is it possible to systematically reprogram or modulate all older cells to function as they once did, perhaps bridging the gap between the old and the young at an organismal level? The data here answer with a rousing, if preliminary, yes, though caveats remain. The tested mice exhibited improvements reminiscent of the leap from a geriatric stage to an extended middle age, but not an indefinite suspension of aging. Even the name Senoreverse conjures a sense that we can spin the arrow of time backwards for cells, though no approach can fully disregard the finite nature of biology. The authors address that an indefinite extension of the natural lifespan is not the conclusion to be drawn here. Instead, the therapy slowed or partly reversed the pathological aspects of senescence, enabling a more extended period of healthy living, as well as some improvement in typical markers of youthfulness.
The question of how well these mice might be protected against new triggers of senescence, be it irradiation or toxins, is also relevant. The capacity to reacquire cell division might ironically invite vulnerabilities if DNA repair capacity is insufficient. The authors found that, thus far, no additional disease burden arose in the long term, yet they note that further assessment in tumor-prone models or more genetically diverse backgrounds is a necessity. We might also wonder whether continued indefinite use of such therapy might cause more subtle tissue-level anomalies, or if a narrower window of partial rejuvenation might be safer. The nuance is that a molecule freeing cells from senescence has the potential to unlock a powerful regenerative force or stir some risk-laden beast inside.
Nevertheless, the reliability of the results stands out, especially with scRNA-seq of the liver and skin in older animals. The transcriptomes show that a previously tiny fraction of dividing cells has expanded under therapy, reshaping the tissue’s cellular identity. Simultaneously, the cluster of heavily senescent cells shrinks. The mechanistic synergy behind this shift is no doubt a mixture of direct changes to SnCs and indirect modifications in the environment, such as reduced proinflammatory cytokines. In synergy, the renewed SnCs might produce signals that further encourage healthy cells to proliferate or differentiate appropriately.
Such synergy is reminiscent of embryonic influences. Indeed, the authors note that hESC-Exos have a wide variety of beneficial cargo, from RNA-binding proteins to other microRNAs, any of which might cooperate with miR-302b to sustain these reprogramming or reactivation events. The exosomes could conceivably deliver more than just one beneficial microRNA, which might fortify the reacquired proliferation with improved genome stability. For now, the authors confirm that the presence of miR-302b alone is sufficient to account for the rejuvenation in multiple cell culture and in vivo contexts, although further lines of inquiry might isolate other small RNAs or proteins that amplify or refine the effect.
Another highlight from these data is the improved cognition and physical performance in aged mice. Memory and learning tasks in older rodents typically degrade with time, reflecting hippocampal deficits, synapse decline, or generally heightened neuroinflammation. That older mice receiving exosomal therapy or miR-302b performed better in the Morris water maze (a test of spatial learning and memory) or on the rotarod (a measure of motor coordination) underscores how far-reaching the therapy’s benefits appear to be. The enhanced performance suggests that some neurons or glia implicated in the aging brain might also have partially reversed their senescence or at least had inflammatory stresses alleviated. The fact that these exosomes (or miR-302b cargo) cross or circumvent the blood-brain barrier is a complicated matter that warrants deeper investigation. Possibly, changes in peripheral tissues and systemic inflammation suffice to improve brain function, or there might be a more direct effect within neural tissue.
All of this underscores that the significance of these findings is wide-ranging, beyond a simple demonstration that one can forcibly reintroduce old fibroblasts to the cell cycle. Reversing senescence might resonate across various tissues and organ systems, leading to a globally rejuvenated organism. That no major safety concerns arose in mice up to 24 months of therapy is vital for acceptance, though one must keep in mind that mouse models are not always predictive of human complexities. The way forward, presumably, includes refining dosing strategies, thoroughly verifying the long-term genomic and functional integrity of reactivated cells, and investigating potential synergy or conflict with other rejuvenation strategies, such as partial reprogramming or senolytics. The interplay of cell cycle reactivation and immune regulation might also be studied in detail.
In sum, the revelation that exosomal miR-302b delivered to older mice reversed the hallmark signals of senescence and allowed for renewed proliferation is nothing short of remarkable. The synergy of molecular control—especially the suppression of Cdkn1a and Ccng2—unlocks the gate to cell division once more. Observers might well compare this to opening a second act for cells, one in which they are no longer inert bystanders but active contributors to the body’s rejuvenation. The gains in muscle strength, hair regeneration, improved cognition, and extended lifespan all paint a picture of an approach that challenges the inevitability of the slow, inexorable shutdown in older tissues. And the authors emphasize that applying the approach over long intervals did not provoke an unrestrained cell growth or major diseases, underscoring a potential advantage of reactivating SnCs rather than simply eliminating them. That is not to say the approach is free of unanswered questions: possible interactions with tumors, the stability of repeatedly reactivated cells, and the complexities of large-scale production and regulatory acceptance remain. Yet for now, the story stands as an inspiring, viral-level revelation, appealing to both scientific curiosity and public imagination. The phenomenon captured in this study amplifies a deep human desire—achieving an extended youth or at least a more active, fulfilling elder stage. If this approach is further validated, the method could represent a leap in the quest to mitigate the burdens of aging, bridging a once-formidable gap in our knowledge of how to recapture vigor from what was once considered irreversible cellular senescence. The promise is vast, and while the ultimate applications remain an open horizon, the path ahead is fueled by these enthralling data that invite us to consider aging not as a closed door, but as a threshold that may be nudged—at least partly—backwards in time.
Subject of Research: Mammalian aging process and cellular senescence
Article Title : Exosomal miR-302b rejuvenates aging mice by reversing the proliferative arrest of senescent cells
News Publication Date : 15 January 2025
Article Doi References : https://doi.org/10.1016/j.cmet.2024.11.013
Image Credits :Scienmag
Keywords : aging senescence exosomes miR-302b cell proliferation rejuvenation lifespan arrest
What's Your Reaction?