Porcine Heart Transplant
The successful transplantation of a genetically modified porcine heart into a living human marks a significant milestone in the field of xenotransplantation. This innovative procedure represents the culmination of decades of research aimed at overcoming biological and immunological barriers that have long hindered the transplantation of animal organs into humans. Following the lessons learned from […]


The successful transplantation of a genetically modified porcine heart into a living human marks a significant milestone in the field of xenotransplantation. This innovative procedure represents the culmination of decades of research aimed at overcoming biological and immunological barriers that have long hindered the transplantation of animal organs into humans. Following the lessons learned from the first genetically modified porcine heart transplant conducted twenty-one months earlier, this second attempt sought to refine protocols, improve donor selection, and enhance patient outcomes.
The recipient of the second genetically modified porcine heart was a 58-year-old man suffering from severe, progressive, inotrope-dependent heart failure caused by ischemic cardiomyopathy. Despite a history of advanced heart failure therapies, the patient’s severe peripheral and central atherosclerotic vascular disease, coupled with a recent gastrointestinal bleed, rendered him ineligible for standard heart transplantation or durable mechanical circulatory support. After thorough evaluation and preparation, the decision to proceed with the experimental xenotransplantation was made, guided by stringent ethical oversight and informed patient consent.
This groundbreaking procedure utilized a porcine heart with ten specific genetic modifications designed to reduce the risk of immune rejection and minimize other complications. Advances in donor screening protocols played a critical role in mitigating the potential risks associated with zoonotic pathogens, such as porcine cytomegalovirus (PCMV), a factor suspected of contributing to complications in the first case. Comprehensive serological and polymerase chain reaction (PCR) testing ensured that the donor animal was free of latent PCMV and other infectious agents. The heart was preserved using the XVIVO Heart Perfusion System, a state-of-the-art technology that maintained organ viability during the transplantation process.
The patient’s preoperative optimization included meticulous fluid management to address cardiorenal syndrome and improve overall health before the transplant. However, the patient experienced a critical ventricular fibrillation event requiring resuscitation hours before surgery. Despite this setback, the transplant team proceeded with confidence, guided by the improved physiological condition of the patient compared to the first xenotransplant recipient.
The transplant surgery itself was a success. Following implantation, the porcine heart demonstrated excellent initial function, with no need for inotropic support and only minor pacing adjustments to achieve optimal heart rates. Postoperative imaging revealed significant resolution of pulmonary edema and pleural effusions, highlighting the functional improvement provided by the xenograft. However, the patient faced early challenges, including perioperative acute kidney injury and persistent vasoplegia, which were managed with continuous renal replacement therapy and vasopressor support.
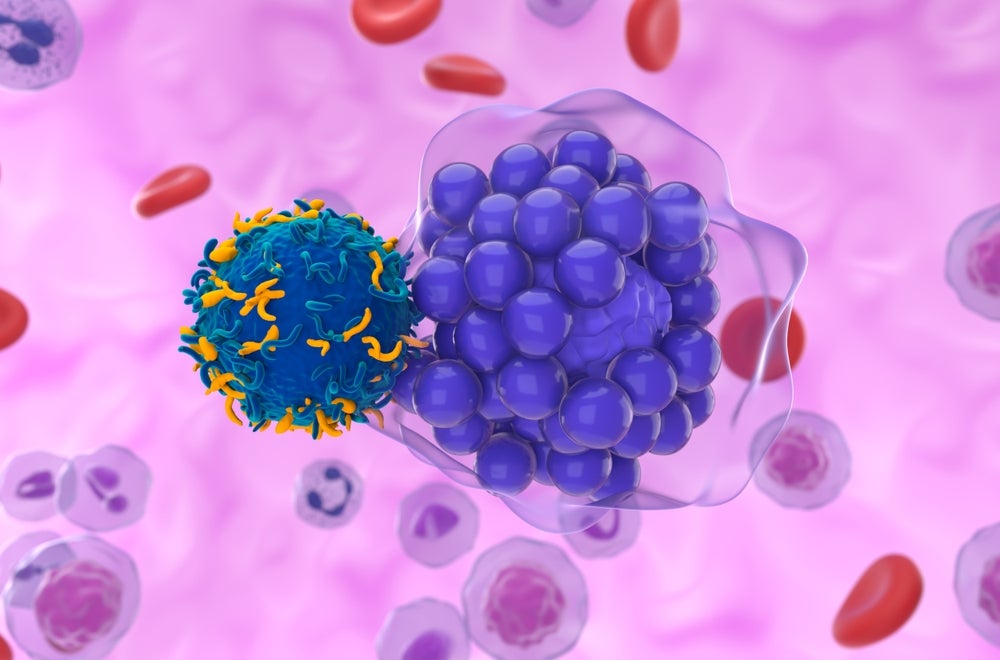
The patient’s post-transplant journey was marked by a series of complex immunological and physiological events. Early echocardiographic assessments showed preserved left ventricular systolic function and robust global longitudinal strain, indicative of healthy graft performance. Yet, the emergence of diastolic dysfunction, biventricular wall thickening, and declining systolic function signaled the onset of graft failure. A comprehensive right heart catheterization confirmed restrictive hemodynamics, while biopsies revealed signs of antibody-mediated rejection (AMR), characterized by endothelial injury, complement deposition, and interstitial edema.
Efforts to counter AMR included therapeutic plasma exchange, complement inhibition with eculizumab, and adjustments to immunosuppressive regimens. Despite these interventions, the patient’s condition deteriorated, necessitating extracorporeal membranous oxygenation (ECMO) by postoperative day 31. Throughout this period, multimodal phenotyping and advanced diagnostics provided invaluable insights into the pathophysiology of xenograft rejection. Notably, donor-derived cell-free DNA (cfDNA) emerged as a sensitive biomarker for early graft injury, underscoring its potential utility in future xenotransplantation monitoring.
Histological examination at autopsy revealed widespread endothelial damage, secondary myocyte ischemia, and progressive fibrosis within the xenograft. These findings, consistent with AMR, underscored the need for enhanced immunosuppressive strategies and further genetic modifications to improve graft resilience. Additionally, the autopsy highlighted the challenges of size mismatches and the potential impact of graft oversizing on functional outcomes.
This second case of porcine-to-human heart transplantation has provided critical insights into the complexities of xenotransplantation. The lessons learned emphasize the importance of precise immunological control, early detection of rejection, and the integration of multimodal diagnostic tools. While the graft ultimately failed after 40 days, the procedure demonstrated the feasibility of porcine heart transplantation as a bridge to life for patients with no other therapeutic options. The patient’s willingness to participate in this experimental endeavor reflects the profound hope that xenotransplantation holds for addressing the global organ shortage.
Future advancements in the field will focus on addressing key challenges identified in this case. Enhancing the genetic engineering of donor animals to include additional complement regulatory proteins, such as CD59, may mitigate the risk of AMR. Optimizing immunosuppressive protocols to achieve therapeutic drug levels earlier in the postoperative course will be crucial. Additionally, developing strategies to reduce the need for blood product transfusions and minimize the risk of passive antibody transfer will enhance patient safety.
This landmark case represents a pivotal step toward the realization of xenotransplantation as a viable clinical therapy. The knowledge gained will inform ongoing research and guide the development of more robust and reliable solutions to extend the survival and improve the quality of life for future recipients. As the field continues to evolve, collaboration among researchers, clinicians, and regulatory bodies will be essential to achieving the full potential of xenotransplantation in transforming organ transplantation and addressing the pressing global demand for donor organs.
Subject of Research: Transplantation of genetically modified porcine hearts into human recipients.
Article Title: Transplantation of a Genetically Modified Porcine Heart into a Live Human
News Publication Date: 08 January 2025
Article Doi References: 10.1038/s41591-025-00123-x
Image Credits: Not provided
Keywords: Xenotransplantation, Porcine Heart Transplant, Genetically Modified Organ, Antibody-Mediated Rejection, Cardiac Failure, Organ Shortage, Immunosuppression, Biopreservation, Donor Screening, Biomedical Innovation
What's Your Reaction?