Peripheral Inflammation’s Role in Parkinson’s Symptoms Explored
A groundbreaking new study published in npj Parkinson’s Disease sheds light on the complex and often unpredictable role that peripheral inflammation plays in the cognitive and symptomatic progression of Parkinson’s disease (PD). Parkinson’s disease, long recognized for its hallmark motor symptoms such as tremor, rigidity, and bradykinesia, is increasingly understood to encompass a broad spectrum […]


A groundbreaking new study published in npj Parkinson’s Disease sheds light on the complex and often unpredictable role that peripheral inflammation plays in the cognitive and symptomatic progression of Parkinson’s disease (PD). Parkinson’s disease, long recognized for its hallmark motor symptoms such as tremor, rigidity, and bradykinesia, is increasingly understood to encompass a broad spectrum of non-motor symptoms, including cognitive impairment, mood disorders, and autonomic dysfunction. The exploration of how systemic inflammation outside the brain influences these outcomes provides a crucial piece in the intricate puzzle of PD pathology.
The research team, led by He, P., Li, Y., Huang, Z., and colleagues, undertook a comprehensive longitudinal and cross-sectional analysis to investigate how peripheral inflammatory markers correlate with variations in cognitive decline and symptomatic severity among individuals diagnosed with Parkinson’s disease. This approach allowed the researchers not only to capture data at a single point but also to observe the dynamic changes and progression over time. Their findings reveal that peripheral inflammation does not affect all patients equally, underscoring the biological heterogeneity inherent to PD.
One of the study’s notable contributions is its detailed profiling of peripheral inflammatory biomarkers and their differential impact on clinical outcomes. Inflammation has been implicated in neurodegeneration, but the mechanisms and extent to which peripheral immune activation crosses the blood-brain barrier and affects central nervous system (CNS) pathology remain incompletely understood. By measuring circulating cytokines, chemokines, and acute-phase proteins, the researchers were able to draw correlations with cognitive performance metrics and motor symptom scales, revealing nuanced relationships.
.adsslot_ZDieQ2lHpN{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_ZDieQ2lHpN{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_ZDieQ2lHpN{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
Importantly, the study highlighted that certain pro-inflammatory cytokines were associated with more rapid cognitive decline in a subset of PD patients. Cognitive impairment in PD ranges from mild cognitive dysfunction to Parkinson’s disease dementia, severely affecting patients’ quality of life. Understanding how systemic inflammatory processes contribute to this decline suggests potential for targeted anti-inflammatory strategies that may slow or alter the disease course, thus offering new therapeutic avenues.
The inflammatory impact on motor symptoms was shown to be variable and not uniformly detrimental. In some cases, elevated peripheral inflammation correlated with exacerbations of motor dysfunction, while in others, no significant association was found. This variability suggests that inflammation interacts with other pathological processes or genetic factors in complex ways. The researchers propose that stratifying patients by inflammatory profiles may improve personalized treatment approaches, especially as inflammation-modulating drugs are increasingly explored in clinical trials.
The methodology utilized in the study incorporated both cross-sectional snapshots of a large PD cohort and repeated measures over extended periods, providing robust evidence for differential inflammatory influences. Advanced statistical modeling enabled the researchers to account for confounding factors such as age, disease duration, medication status, and comorbidities. This rigorous analytic framework strengthens the validity of their conclusions and highlights the importance of considering individual patient contexts in PD research.
Moreover, the study’s longitudinal design provided insights into temporal dynamics — for example, whether bursts of peripheral inflammation might precede or coincide with exacerbations in symptoms. Understanding these temporal relationships deepens our grasp of PD’s pathophysiology and may guide timely interventions. It also raises intriguing questions about the bidirectional relationship between central neuroinflammation and peripheral immune activation.
From a mechanistic standpoint, inflammation-induced disruption to the blood-brain barrier and microglial activation within the brain appear to mediate at least part of the cognitive deficits observed. Microglia, the resident immune cells of the CNS, can become chronically activated under inflammatory conditions, contributing to neuronal dysfunction and loss. However, the degree of peripheral inflammation necessary to trigger such central responses differs among patients, suggesting individual thresholds or protective factors that modulate disease trajectory.
The researchers also emphasized the interplay between peripheral inflammation and alpha-synuclein pathology, a hallmark of PD characterized by protein aggregation in neurons. Inflammatory mediators may facilitate alpha-synuclein propagation or exacerbate its toxicity, further driving neurodegeneration. This link offers a fresh perspective on how systemic immune status influences classical PD pathological mechanisms and calls for comprehensive biomarker panels combining inflammatory and proteinopathy indicators.
Clinically, the findings reinforce the need to monitor inflammatory markers as part of routine assessments in PD management. While inflammation itself may not be the primary cause of PD pathology, it evidently modulates disease expression and progression. This realization supports integrating immunomodulatory considerations into therapeutic strategies, whether through lifestyle modifications, pharmacological agents, or adjunct therapies aimed at reducing systemic inflammation.
The study also draws attention to potential environmental and lifestyle factors that could contribute to peripheral inflammation, such as infections, diet, and chronic stress. Understanding how these elements interact with genetic susceptibility and disease pathology could identify modifiable risk factors and preventive measures. Future research building on these findings may explore how interventions targeting inflammation impact long-term clinical outcomes in PD.
Importantly, this work pioneers a shift away from viewing Parkinson’s disease as a purely neurocentric disorder. Instead, it contextualizes PD within a broader systemic framework, where peripheral immune dysregulation plays a pivotal yet variable role. This systemic approach aligns with emerging paradigms in neurodegeneration research that emphasize the interconnectedness of multiple organ systems and biological pathways.
Given the complexity uncovered, the authors recommend that future clinical trials for PD therapeutics stratify participants based on inflammatory status to better evaluate treatment efficacy. Such stratification could identify responder subgroups and minimize heterogeneity-driven noise in trial results. Additionally, combining anti-inflammatory therapies with standard dopaminergic treatments might prove synergistic, particularly for patients exhibiting high inflammatory burdens.
This study’s implications extend beyond Parkinson’s disease, offering a model for investigating how peripheral immune factors influence cognitive and neurological disorders more generally. Inflammation has been implicated in Alzheimer’s disease, multiple sclerosis, and other neurodegenerative conditions. Therefore, deciphering immune-neural interactions in PD can accelerate understanding across neurological disciplines.
In summary, He, P., Li, Y., Huang, Z., and their team have delivered a pivotal contribution to Parkinson’s disease research by demonstrating that peripheral inflammation’s impact on cognitive and symptomatic outcomes is highly variable and context-dependent. Their work challenges simplified notions of inflammation’s role and advocates for precision medicine approaches that consider immune profiles alongside classical neurological assessments. As the PD field moves forward, integrating immune biology into both research and clinical practice promises to unlock new opportunities for patient-tailored interventions and improved prognostication.
This seminal analysis in npj Parkinson’s Disease offers hope that by harnessing knowledge about peripheral inflammation and its intricate influence on PD, clinicians and researchers can better predict disease trajectories, mitigate cognitive decline, and ultimately enhance the quality of life for individuals living with Parkinson’s disease.
Subject of Research: The variable impact of peripheral inflammation on cognitive decline and symptomatic progression in Parkinson’s disease through longitudinal and cross-sectional analyses.
Article Title: Peripheral inflammation’s variable impact on cognitive and symptomatic outcomes in Parkinson’s disease: a longitudinal and cross-sectional analysis.
Article References:
He, P., Li, Y., Huang, Z. et al. Peripheral inflammation’s variable impact on cognitive and symptomatic outcomes in Parkinson’s disease: a longitudinal and cross-sectional analysis. npj Parkinsons Dis. 11, 155 (2025). https://doi.org/10.1038/s41531-025-01019-7
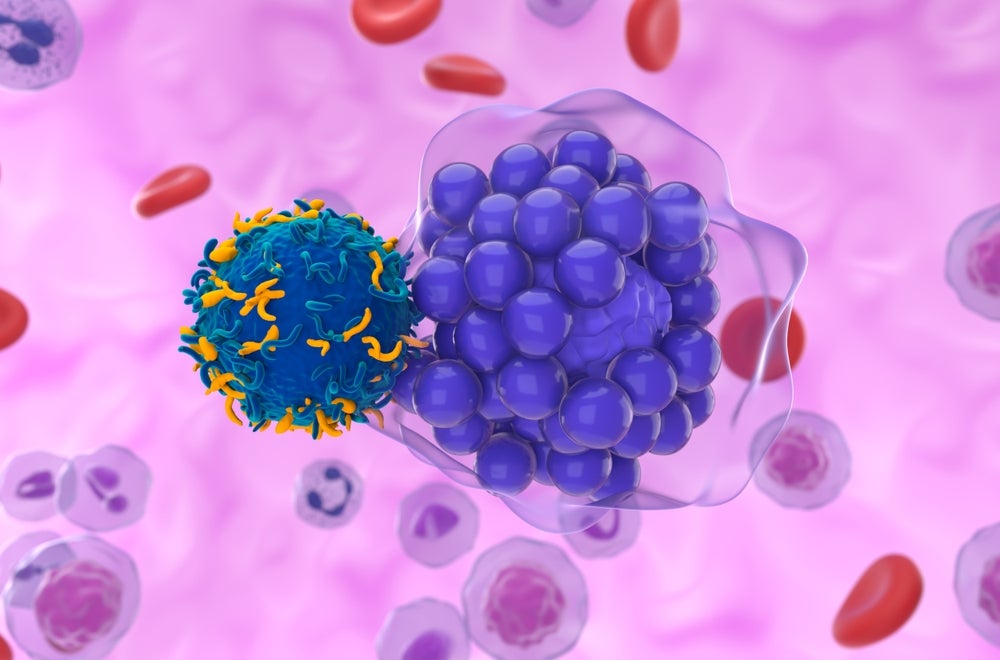
Image Credits: AI Generated
Tags: autonomic dysfunction in Parkinson’s diseasebiological heterogeneity in Parkinson’sbiomarkers of inflammation in Parkinson’scognitive symptoms in PDimpact of inflammation on Parkinson’s progressionlongitudinal study on Parkinson’s diseasemood disorders in Parkinson’s patientsmotor and non-motor symptoms of Parkinson’sParkinson’s disease research findingsperipheral inflammation in Parkinson’s diseaserole of inflammation in neurodegenerationsystemic inflammation and cognitive decline
What's Your Reaction?