Neoadjuvant Immunotherapy for early stage melanoma shows positive results
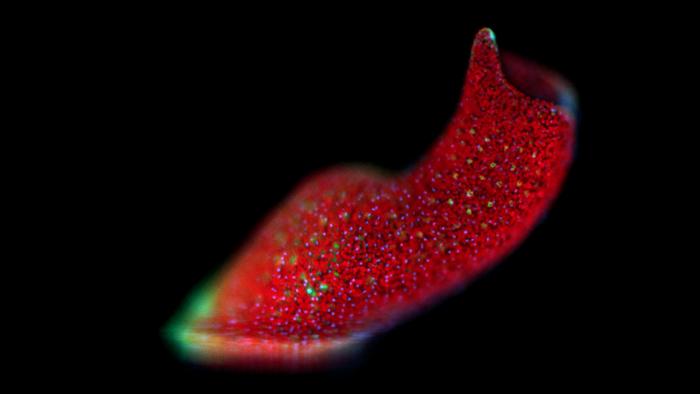
Immunotherapy before surgery for patients with metastatic melanoma appears to be especially successful. Fifty-nine percent of patients responds so well to this therapy that adjuvant treatment is no longer needed, according to the results of the NADINA study that were published today. Credit: Netherlands Cancer Institute Immunotherapy before surgery for patients with metastatic melanoma appears […]
Immunotherapy before surgery for patients with metastatic melanoma appears to be especially successful. Fifty-nine percent of patients responds so well to this therapy that adjuvant treatment is no longer needed, according to the results of the NADINA study that were published today.
Credit: Netherlands Cancer Institute
Immunotherapy before surgery for patients with metastatic melanoma appears to be especially successful. Fifty-nine percent of patients responds so well to this therapy that adjuvant treatment is no longer needed, according to the results of the NADINA study that were published today.
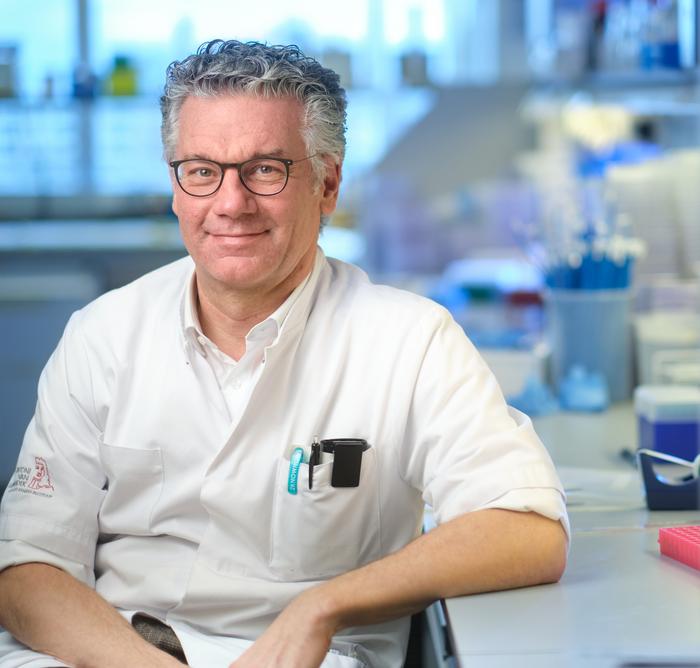
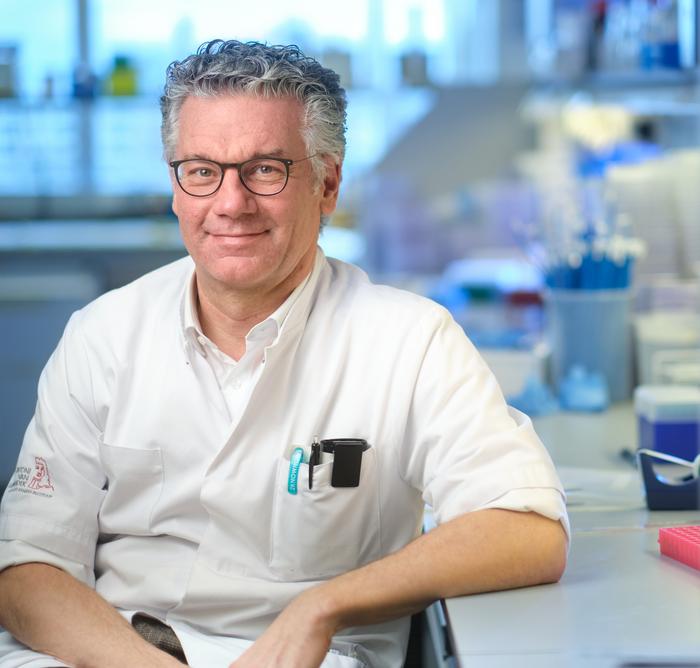
The NADINA study, led by researchers from the Netherlands Cancer Institute, was named one of the eleven clinical studies with the biggest impact on health care in 2024 by Nature Medicine. The study now proves that this was not an empty claim, as shown by the results presented by medical oncologist and research leader Christian Blank today during ASCO 2024, the international congress of the American Society of Clinical Oncology in Chicago. The results have also been published in New England Journal of Medicine (NEJM).
Long lead-up
Standard treatment for patients with metastatic skin cancer (melanoma stage III) consists of the removal of the local lymph nodes, followed by a year of adjuvant treatment with immunotherapy or targeted therapy. “Despite that, we still see disease recurrence within three to five years in nearly half of these patients,” Blank explains. That’s why he setup the OpACIN trial ten years ago, in which immunotherapy before surgery (neoadjuvant immunotherapy) was compared to immunotherapy after surgery (adjuvant therapy). The study showed that neoadjuvant immunotherapy could induce a stronger and broader immune response against the tumor, at the cost of more side effects. Blank: “That’s why we initiated the OpACIN-neo trial, comparing three schedules with varying doses and eventually finding a safe and effective schedule. In the subsequent PRADO trial, we applied this optimal dose to 99 patients. The patients who responded well to the treatment were able to forgo surgery and adjuvant treatment.”
In 2022, Blank and his research group published the results of the PRADO study, in which 60 out of 99 patients with metastatic melanoma responded well to immunotherapy before surgery. “Conducting these studies eventually led to the design of the NADINA trial, the first phase 3 trial investigating neoadjuvant checkpoint inhibition for early stage melanoma,” Blank states.
High response rate
In the international investigator initiated NADINA trial, 423 patients were randomized to two groups: the first group received two immunotherapy treatments with ipilimumab and nivolumab, followed by surgery. The second group received standard treatment involving surgery followed by 12 rounds of immunotherapy with nivolumab. “In 59% of patients who had received immunotherapy before surgery, the tumor was nearly entirely or completely gone, which meant that they did not require additional treatment.” Even people who did not respond well to the therapy and had an unfavorable prognosis benefited from the therapy: they were able to start adjuvant treatment with immunotherapy or targeted therapy after surgery.
Effective and cost-efficient
The effects of the treatment become apparent quickly. After one year, almost 84% of patients who had received neoadjuvant treatment were still tumor-free, compared to 57% of the group receiving standard treatment. Blank: “Patients whose tumors were nearly entirely or completely gone, saw even better results; 95% remained tumor-free, after only six months of treatment.” 76% of patients whose tumors were only partially gone were still tumor-free one year after the start of their treatment, compared to 57% of patients who did not respond well to neoadjuvant therapy. These two patient groups received additional adjuvant treatment after their neoadjuvant treatment and surgery. In three years, the researchers expect to know whether this positive trend continues and could improve survivorship. The next challenges in this field will be to improve treatment outcomes of patients who responded less favorably.
Besides a greater chance of tumor-free survival, most patients were able to cut down their treatment time to only six weeks. Blank: “Treatment is a lot cheaper – €16,000 instead of €68,000, which would free up about 30 to 40 million euros in the Netherlands, and could reach a billion euros worldwide.”
The treatment still needs to be registered and approved in the Netherlands to qualify for health care insurance coverage. That’s why it will not be immediately available. Blank: “We are talking with various public authorities to ensure that the treatment can eventually receive coverage.”
Personalized medicine
There are many studies looking into neoadjuvant treatments for various cancer types, including lung cancer, bladder cancer, and breast cancer. “These trials often combine a neoadjuvant approach with standard adjuvant treatment after surgery, instead of adapting treatment to the response to the neoadjuvant part,” Blank explains. “The NADINA trial is the very first trial within the oncological field that researched a purely immune-therapeutic and personalized treatment. Eventually we aspire to be able to provide personalized immunotherapy by reading out the tumor RNA in every individual patient, and providing a treatment that we know works best based on the results.”
Journal
New England Journal of Medicine
Method of Research
Randomized controlled/clinical trial
Subject of Research
People
Article Title
Neoadjuvant nivolumab and ipilimumab in resectable stage III melanoma
Article Publication Date
2-Jun-2024
What's Your Reaction?