Nationwide Study on Biologic Treatments for Pediatric Eosinophilic Esophagitis
In an era where precision medicine is rapidly transforming pediatric healthcare, a groundbreaking nationwide study has emerged, shedding light on the utility of biological treatments in children suffering from eosinophilic esophagitis (EoE). Published in Pediatric Research in 2025, this comprehensive investigation led by Soudant, Lejeune, Aumar, and their colleagues delves into an intricate analysis of […]


In an era where precision medicine is rapidly transforming pediatric healthcare, a groundbreaking nationwide study has emerged, shedding light on the utility of biological treatments in children suffering from eosinophilic esophagitis (EoE). Published in Pediatric Research in 2025, this comprehensive investigation led by Soudant, Lejeune, Aumar, and their colleagues delves into an intricate analysis of the clinical efficacy, safety, and long-term outcomes associated with biologic therapeutics applied across diverse pediatric populations afflicted by this chronic, immune-mediated disease.
Eosinophilic esophagitis, a formidable chronic inflammatory condition characterized by eosinophilic infiltration of the esophageal mucosa, has vexed clinicians and researchers alike due to its complex pathophysiology and variable clinical presentation. Prior to the advent of targeted biological interventions, treatment paradigms largely relied on dietary modifications, proton pump inhibitors, and topical corticosteroids, approaches often fraught with suboptimal efficacy, poor patient adherence, and considerable relapse rates. The investigation presented by Soudant et al. capitalizes on recent advancements in immunology and molecular medicine to elucidate how novel biologic agents, which specifically inhibit key inflammatory mediators, hold transformative potential for this vulnerable pediatric cohort.
This nationwide experience involved meticulous data collection from multiple tertiary referral centers, encompassing a comprehensive array of pediatric patients systematically treated with a spectrum of biologic agents, including monoclonal antibodies targeting IL-5, IL-13, and other pivotal cytokines implicated in EoE pathogenesis. The study’s rigorous methodology combined prospective observational data with retrospective analyses, facilitating a granular evaluation of clinical endpoints such as symptom resolution, histological remission, and quality of life metrics. Notably, the study’s scale and diversity lend unprecedented generalizability to its conclusions, addressing a significant knowledge gap in pediatric EoE management.
.adsslot_LQHRe2EO80{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_LQHRe2EO80{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_LQHRe2EO80{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
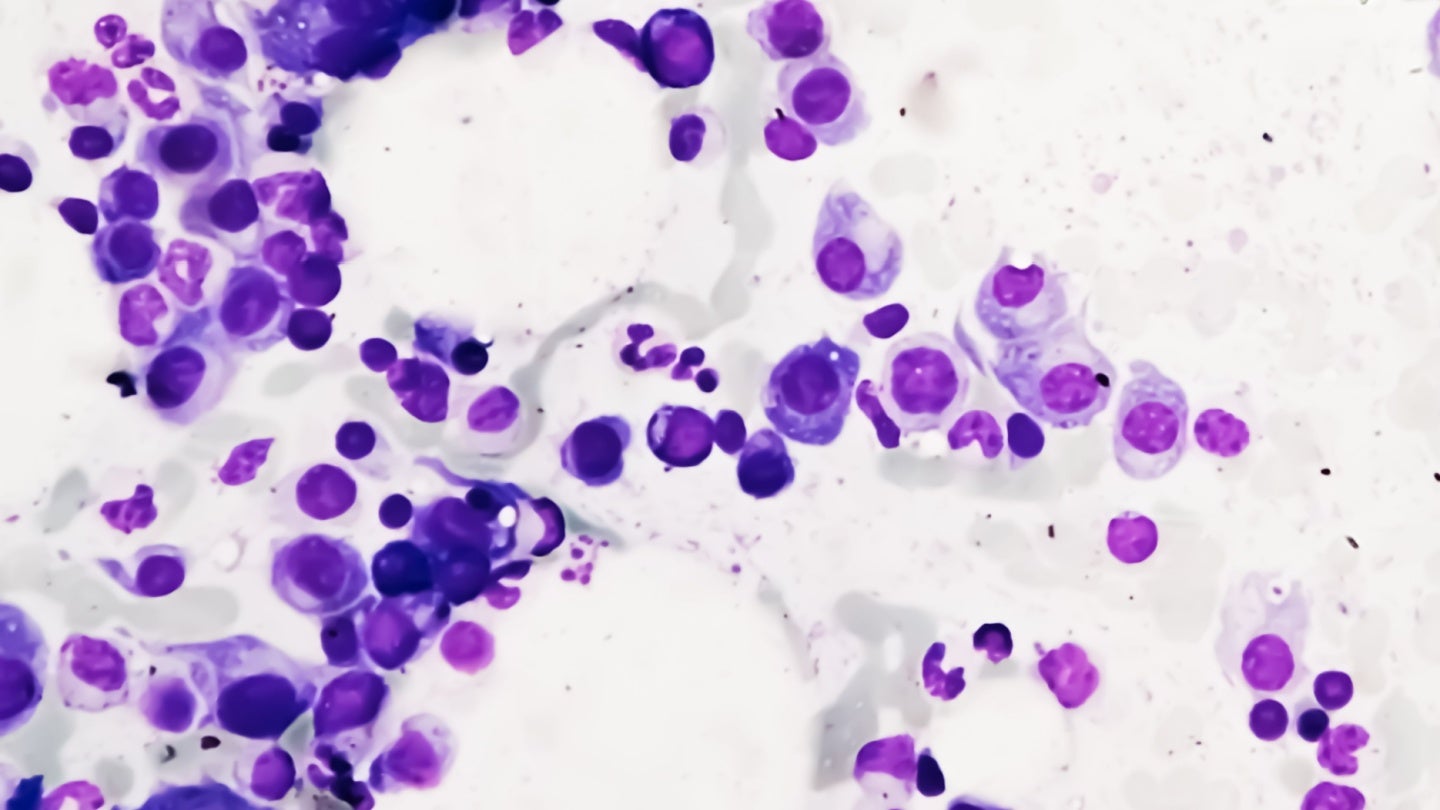
Understanding the immunological underpinnings of eosinophilic esophagitis is paramount to appreciating the revolutionary impact of these biologics. EoE is distinguished by a dysregulated Th2-type immune response, precipitating eosinophil recruitment and activation within the esophageal epithelium. This inflammatory cascade leads to tissue remodeling, fibrosis, and subsequently, dysphagia and esophageal dysfunction. Traditional therapies largely target surface-level inflammation; however, biologics interfere with the upstream signaling pathways, neutralizing key cytokines such as IL-5, which orchestrates eosinophil survival and activation, and IL-13, which perpetuates epithelial barrier dysfunction and fibrosis.
The therapeutic interventions assessed comprised biologics with distinct mechanisms of action—anti-IL-5 agents such as mepolizumab and reslizumab, and anti-IL-13 agents including dupilumab, each systematically evaluated for efficacy and safety profiles in pediatric subjects. The study’s longitudinal design enabled the tracking of response durability, immunogenicity concerns, and adverse event profiles over a span of multiple treatment cycles. Strikingly, a substantial proportion of children achieved both symptomatic relief and histologic remission, underscoring the potential to modify disease trajectory rather than merely palliate symptoms.
One of the pivotal aspects emphasized in this nationwide study is the heterogeneity of patient responses, spotlighting the salient need for personalized therapeutic regimens. Biomarker analyses integrated within the research framework revealed differential cytokine expression and eosinophilic activity that correlated with varied therapeutic outcomes. This precision medicine approach heralds a future where biomarker profiling could tailor biologic selection, optimizing efficacy while minimizing unnecessary exposure and side effects.
Safety considerations remain at the forefront of pediatric biological therapy deployment. The study meticulously cataloged adverse effects, ranging from mild injection site reactions to rare systemic immunosuppression complications. Crucially, no significant increase in serious adverse events was observed compared to conventional therapies, cementing a reassuring safety profile vital for chronic pediatric conditions necessitating sustained immunomodulation.
The socio-economic implications of introducing expensive biologics also surfaced within the study’s comprehensive discourse. By evaluating healthcare utilization patterns, hospitalization rates, and indirect costs post-therapy initiation, the researchers provided a multi-dimensional cost-benefit analysis. Early evidence suggests that despite higher upfront costs, biologic treatments may reduce long-term healthcare burdens by decreasing disease exacerbations and improving overall patient quality of life.
Moreover, this national-scale investigation explored the psychosocial dynamics associated with pediatric EoE and its treatment. Chronic diseases exert profound psychological impacts, especially in children navigating developmental milestones. The study incorporated patient-reported outcomes indicating improved mental health indices and social functioning following successful biologic therapy, highlighting the holistic benefits beyond mere physiological remission.
Another remarkable finding pertains to the age stratification of therapeutic effectiveness. Younger children demonstrated rapid clinical improvements, potentially attributable to less entrenched tissue remodeling, while adolescents exhibited variable responses, suggesting that timing of intervention bears critical importance. This stratification challenges clinicians to consider the optimal therapeutic windows for intervention to maximize disease control and prevent irreversible esophageal damage.
The role of multidisciplinary collaboration emerged as a key factor in successful biological therapy implementation. The study underscored coordinated efforts among pediatric gastroenterologists, allergists, immunologists, dietitians, and nursing teams to monitor response, manage side effects, and tailor supportive care, ensuring comprehensive patient management. Such models of care reinforce the paradigm shift from symptom-focused treatment to integrated disease modification strategies.
Furthermore, this nationwide experience inherently raises important research questions for future trials, including long-term immunological sequelae, the impact of biologics on esophageal remodeling reversal, and the exploration of novel targets within the EoE inflammatory cascade. It also brings forth ethical considerations regarding equitable access to these cutting-edge therapies, especially in resource-limited settings, thereby stimulating dialogue on healthcare policy and funding priorities.
In synthesis, the study by Soudant et al. represents a watershed moment in pediatric eosinophilic esophagitis management, illustrating how the confluence of immunological insight and biotechnological innovation can recast the therapeutic landscape of chronic pediatric diseases. By demonstrating tangible clinical benefits, acceptable safety profiles, and real-world applicability, this nationwide experience paves the way for future standard-of-care revisions that prioritize biologics as frontline interventions.
As the global pediatric healthcare community grapples with increasing rates of eosinophilic esophagitis, driven by environmental and genetic factors, such comprehensive evidence-based evaluations are indispensable. They empower clinicians to make informed treatment decisions that transcend symptom control, aiming instead for true disease remission and improved lifelong outcomes for affected children.
Looking ahead, continued research efforts and real-world data collection will be vital to refine patient selection criteria, optimize dosing regimens, and assess long-term durability of biological treatments. The promise held by these agents is immense, with the potential not only to mitigate current disease burden but to alter the natural history of eosinophilic esophagitis entirely.
In conclusion, this seminal investigation signifies a bright horizon for pediatric EoE management, where targeted biological therapies can deliver precision medicine tailored to individual immunological profiles, transforming lives and setting new standards in chronic inflammatory disease care.
Subject of Research: Nationwide evaluation of biological treatments in pediatric eosinophilic esophagitis.
Article Title: A nationwide experience of biological treatments in children with eosinophilic esophagitis.
Article References:
Soudant, J., Lejeune, S., Aumar, M. et al. (2025). A nationwide experience of biological treatments in children with eosinophilic esophagitis. Pediatr Res. https://doi.org/10.1038/s41390-025-04011-2
Image Credits: AI Generated
DOI: https://doi.org/10.1038/s41390-025-04011-2
Tags: biologic treatments for pediatric eosinophilic esophagitischronic inflammatory diseases in childrenclinical efficacy of biologic therapies in childrendietary modifications for eosinophilic esophagitiseosimmunology advancements in EoE treatmentlong-term outcomes of eosinophilic esophagitis treatmentspatient adherence to EoE treatment plansprecision medicine in pediatric healthcareproton pump inhibitors in pediatric EoE managementsafety of biologic therapies for EoE
What's Your Reaction?