Mobile teams bring COVID-19 vaccines to rural villages in Sierra Leone
URBANA, Ill. – COVID-19 vaccination rates remain low in many African countries, often because providing access to vaccines is difficult in remote areas. A new international research project showed that intervention with mobile vaccination teams in Sierra Leone is an effective way of reaching rural populations to increase vaccination uptake. Credit: Madison Levine URBANA, Ill. […]

URBANA, Ill. – COVID-19 vaccination rates remain low in many African countries, often because providing access to vaccines is difficult in remote areas. A new international research project showed that intervention with mobile vaccination teams in Sierra Leone is an effective way of reaching rural populations to increase vaccination uptake.

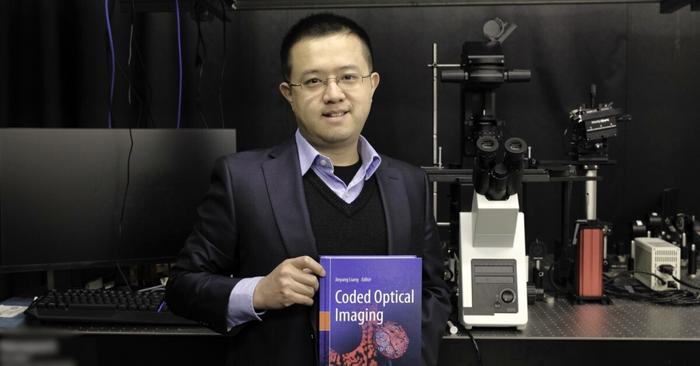
Credit: Madison Levine
URBANA, Ill. – COVID-19 vaccination rates remain low in many African countries, often because providing access to vaccines is difficult in remote areas. A new international research project showed that intervention with mobile vaccination teams in Sierra Leone is an effective way of reaching rural populations to increase vaccination uptake.
Madison Levine, a doctoral student in the Department of Agricultural and Consumer Economics (ACE), part of the College of Agricultural, Consumer and Environmental Sciences (ACES) at the University of Illinois Urbana-Champaign, participated in the project as a field research assistant. She is a co-author on the research paper, which is published in Nature, and she shared her experiences overseeing the project implementation.
“I was organizing the fieldwork, coordinating communications, and training everybody. Everything was approved by the principal investigators, of course, but I was making field plans and ensuring every route would work within the time frame we had. I assisted if there were any problems, and I was in as many villages as possible,” Levine said.
“It was challenging because we were going to very remote areas. We had a car for the project, but there were places you couldn’t go by car, so there was a lot of traveling on motorbikes, and sometimes we had to take a boat to get across an area of water. The health staff who were going with us carried the vaccines in ice boxes.”
Levine holds a master’s degree in international development economics from the University of San Francisco and she worked in Sierra Leone for several years before implementing the COVID-19 project. At Illinois, her advisors are ACE professors Hope Michelson and Sarah Janzen.
The research was conducted by a collaborative team from the International Growth Centre, University of Oxford, Yale University, and Wageningen University in cooperation with the Sierra Leone Ministry of Health and Sanitation (MoHS) and the international non-governmental organization Concern Worldwide. The Sierra Leone MoHS operates a network of peripheral health units, but many Sierra Leoneans live far away from these units, and people have to travel an average of 3.5 hours each way to reach a vaccination center.
The study included 150 rural villages in Sierra Leone that were located more than 5 miles from any health unit, and the intervention took place over several days.
“First, a team of community mobilizers would talk to the village leaders. Once the leaders approved, the team would hold a public meeting where they would talk about what the vaccine does and address any concerns. The next day, they would put up a small clinic with a couple of tables that held the medical supplies, and people would line up to get vaccinated. The MoHS assisted in providing trained nurses and medical staff for each place. All teams included local people who spoke the language of the village, which helped to build trust,” Levine said.
“The majority of the communities welcomed our team. These very small villages are used to being surpassed by bigger cities, so they were happy we were coming out to them. Only two villages declined to participate, and we had to respect that.”
The study found that immunization rates increased by about 26% in the trial villages. In addition, people who were traveling nearby would also stop to get vaccinated, further increasing the uptake. On average, the cost was about $33 per person, making it a very cost-effective intervention.
While there is some misinformation and vaccine hesitancy, by far the biggest obstacle is vaccine access, Levine said. “This project clearly shows you can make it cost-effective to reach people, even in very remote areas. For instance, the COVID-19 vaccine was received for free, so there needs to be a process in place to distribute it. It has to be budgeted properly and organized well, which people are highly capable of doing. This project shows it can be done, and hopefully, it opens doors for future global health interventions.”
The paper, “Last-mile delivery increases vaccine uptake in Sierra Leone,” is published in Nature [DOI:10.1038/s41586-024-07158-w]
Journal
Nature
DOI
10.1038/s41586-024-07158-w
Method of Research
Randomized controlled/clinical trial
Subject of Research
People
Article Title
Last-mile delivery increases vaccine uptake in Sierra Leone
Article Publication Date
13-Mar-2024
What's Your Reaction?