Innovative Approach for Administering Cell Therapies to Critically Ill Patients on External Lung Support
In a groundbreaking advancement within the realm of regenerative medicine and critical care, a team of multidisciplinary scientists led by Professor Bernat Soria at the Miguel Hernández University of Elche (UMH) in Spain has unveiled a novel technique to administer stem cell therapies in patients reliant on extracorporeal membrane oxygenation (ECMO). This method, termed Consecutive […]


In a groundbreaking advancement within the realm of regenerative medicine and critical care, a team of multidisciplinary scientists led by Professor Bernat Soria at the Miguel Hernández University of Elche (UMH) in Spain has unveiled a novel technique to administer stem cell therapies in patients reliant on extracorporeal membrane oxygenation (ECMO). This method, termed Consecutive Intrabronchial Administration (CIBA), offers an innovative solution to a persistent clinical conundrum: delivering reparative cellular therapies to the lungs of critically ill patients supported by ECMO, whose fragile physiologies have precluded conventional intravenous approaches.
ECMO, an advanced life-support system, temporarily assumes the role of the lungs and heart by oxygenating the blood outside the body, effectively providing a bridge to recovery or transplantation in cases of severe respiratory failure. While ECMO sustains life, it simultaneously complicates therapeutic interventions, especially those involving intravenous cell infusions. Traditional systemic administration of mesenchymal stromal cells (MSCs) risks obstructing the delicate gas-exchange membranes of the ECMO circuit, potentially jeopardizing the system’s function and, consequently, patient survival. Until now, this hazard has largely barred the exploration of stem cell therapies in this vulnerable patient group.
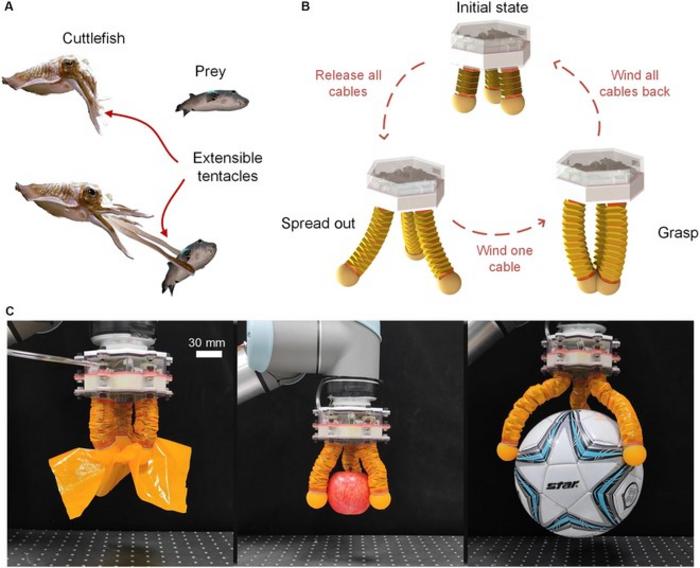
The CIBA method creatively circumvents this barrier by employing a bronchoscope—a slender, flexible tube inserted directly into the airways—to deliver stem cells precisely into the pulmonary alveoli. This targeted, fractionated intrabronchial administration bypasses the bloodstream and the ECMO circuit, ensuring that the therapeutic cells reach the damaged lung tissue without compromising the extracorporeal oxygenation machinery. This controlled, localized delivery maximizes therapeutic potential while safeguarding the integrity of life support, an achievement deemed a technical milestone in critical care medicine.
At the cellular level, the therapeutic agents are Wharton’s jelly-derived mesenchymal stromal cells (WJ-MSCs), known for their immunomodulatory and regenerative properties. Unlike specialized lung cells, these MSCs possess plasticity that allows them to migrate into damaged tissue, modulate inflammatory responses, and promote tissue repair. Upon reaching the alveolar spaces, these cells engage with resident immune populations—including alveolar macrophages and regulatory T cells—stimulating the release of anti-inflammatory cytokines such as interleukin-10 (IL-10) while attenuating pro-inflammatory cytokines like tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6). This nuanced immunological interaction helps modulate the excessive lung inflammation characteristic of end-stage lung diseases and severe respiratory distress.
The initial application of the CIBA technique was carried out under compassionate use in a critically ill two-year-old patient suffering from end-stage interstitial lung disease, a devastating condition marked by progressive scarring and respiratory compromise that left no option for lung transplantation. Despite prolonged ECMO support and aggressive immunosuppression, the child’s condition showed minimal improvement. Following regulatory approval by the Spanish Agency of Medicines and Medical Devices (AEMPS), clinicians administered a carefully titrated single dose of WJ-MSCs via the CIBA method. Remarkably, the procedure was well tolerated with no immediate adverse effects, and the patient was successfully extubated within 72 hours—a promising sign of clinical stability.
Although the child’s ultimate clinical course culminated in withdrawal of ECMO support after 127 days due to irreversible progression, this pioneering case demonstrated, for the first time, the feasibility and safety of delivering stem cell therapies directly into the lungs during ECMO support. This breakthrough paves the way for expanded research and clinical trials to explore repeated dosing regimens, dose optimization, and long-term efficacy in larger cohorts.
Technically, the CIBA procedure represents a synthesis of pulmonology, bioengineering, and cell therapy. The delicate act of “drip-feeding” MSCs into the alveolar spaces demands precise control over cell suspension volume, distribution timing, and delivery pressure to prevent airway injury or inadvertent redistribution into the systemic circulation. Professor Soria likens the technique metaphorically to watering a fragile plant with the gentlest possible drip, ensuring nourishment without flooding. This analogy emphasizes the finesse required when working with severely compromised lungs under ECMO.
Scientifically, this research addresses an unmet need in the treatment of respiratory failure complicated by critical illness and advanced life support. Intravenous administration of stem cells has been explored for diverse pulmonary conditions but remained impractical in ECMO patients due to technical risks. By circumventing these risks, the CIBA method opens a new therapeutic avenue rooted in regenerative medicine that might complement or even enhance existing ECMO protocols.
This safety and feasibility study constitutes a proof-of-concept investigation under the DECODE clinical project, funded by Spain’s Instituto de Salud Carlos III. The collaborative effort engaged 28 clinicians spanning four premier Spanish institutions—including Hospital 12 de Octubre in Madrid, Banc de Sang i Teixits in Catalonia, the Institute of Bioengineering at UMH, and the Institute for Health and Biomedical Research of Alicante (ISABIAL)—reflecting a concerted national commitment to translational science with tangible clinical impact.
Notably, the team behind CIBA has chosen not to pursue patent protection for the technique. This open-science approach aims to remove financial barriers, facilitating rapid dissemination and adoption of CIBA within public healthcare systems globally. Given the escalating costs of advanced therapies, this decision underscores an ethical commitment to equitable healthcare access and innovation sharing.
The biological rationale for intrabronchial MSC delivery benefits from an intricate understanding of pulmonary immunology and regenerative mechanisms. MSCs sourced from Wharton’s jelly in the umbilical cord offer advantages due to their relative abundance, ease of harvesting, low immunogenicity, and potent immunomodulatory effects compared to other MSC sources like bone marrow or adipose tissue. Concentrating these cells directly in the lungs postulates augmented local effects, including amelioration of alveolar epithelial damage, inhibition of fibrotic pathways, and restoration of vascular integrity, processes critical in end-stage pulmonary diseases.
Looking ahead, comprehensive randomized controlled trials will be necessary to validate CIBA’s efficacy, optimize dosing protocols, and assess long-term safety. Explorations into repeated administrations and combining MSC therapy with adjunct treatments may yield synergistic benefits. Moreover, extending this methodology to adult patients and diverse pulmonary pathologies could revolutionize regenerative strategies in critical care.
In summary, the CIBA technique represents a remarkable convergence of clinical innovation and biomedical science, overcoming formidable technical challenges to deliver life-sustaining cell therapies directly where they are most needed. As critical care medicine continues to grapple with the complexities of respiratory failure, interventions like CIBA herald a new era in which regenerative medicine can be safely integrated into life-supporting platforms, ultimately improving outcomes for the most vulnerable patients.
Subject of Research: People
Article Title: Consecutive intrabronchial administration of Wharton’s jelly-derived mesenchymal stromal cells in ECMO-supported pediatric patients with end-stage interstitial lung disease: a safety and feasibility study (CIBA method)
News Publication Date: 5-Apr-2025
Web References: http://dx.doi.org/10.1186/s13287-025-04289-3
References: CIBA Method and the Rationale for MSC Administration. Stem Cell Res Ther. 2025. doi: 10.1186/s13287-025-04289-3
Image Credits: CIBA Method and the Rationale for MSC Administration. Stem Cell Res Ther. 2025. doi: 10.1186/s13287-025-04289-3
Keywords: Respiratory failure, Stem cell therapy, Medical tests, Pulmonary alveoli
Tags: bronchoscope-assisted cell deliverycellular therapies in ECMO patientsConsecutive Intrabronchial Administrationcritical care advancementsECMO for critically ill patientsextracorporeal membrane oxygenationlung repair therapiesmesenchymal stromal cells administrationmultidisciplinary approach in medicineregenerative medicine innovationsstem cell therapiestherapeutic interventions in respiratory failure
What's Your Reaction?