Hypoxia Boosts MS via Macrophage Inflammasome Activation
In an unprecedented leap forward in our understanding of multiple sclerosis (MS) pathology, recent research elucidates a critical mechanism by which hypoxic conditions exacerbate disease progression. The intricate work spearheaded by Okano, Ashida, Tsukasaki, and colleagues delves into the synergistic relationship between low oxygen levels, macrophage inflammasome activation, and chronic infection by the periodontal pathogen […]


In an unprecedented leap forward in our understanding of multiple sclerosis (MS) pathology, recent research elucidates a critical mechanism by which hypoxic conditions exacerbate disease progression. The intricate work spearheaded by Okano, Ashida, Tsukasaki, and colleagues delves into the synergistic relationship between low oxygen levels, macrophage inflammasome activation, and chronic infection by the periodontal pathogen Porphyromonas gingivalis. This multifaceted interplay unravels new dimensions in MS progression and offers a tantalizing glimpse into potential therapeutic targets that may transform future interventions for this debilitating neurological disorder.
Multiple sclerosis, a chronic autoimmune disease characterized by progressive demyelination and neuroinflammation within the central nervous system, remains a formidable challenge to clinicians and researchers alike. While genetic and environmental factors have traditionally been implicated in disease susceptibility, emerging evidence highlights the vital role of microenvironmental stressors, such as hypoxia, in modulating immune responses and accelerating neuropathology. The study by Okano et al. represents a paradigm shift, positioning hypoxia not merely as a bystander but as a potent driver of inflammasome activity in immune cells that infiltrate the CNS.
Macrophages, pivotal players in innate immunity, exhibit remarkable plasticity in response to environmental cues. Under normal physiological conditions, these cells maintain tissue homeostasis and assist in clearing pathogens. However, in the hypoxic milieu characterizing inflamed CNS lesions in MS, macrophages undergo profound metabolic and phenotypic reprogramming. The research team demonstrated that hypoxia markedly amplifies the activation of inflammasomes, multiprotein complexes responsible for the maturation and secretion of pro-inflammatory cytokines such as interleukin-1β (IL-1β). This hyperactivation not only fuels the neuroinflammatory cascade but also contributes to tissue damage and demyelination.
.adsslot_sd8GuNBX2q{ width:728px !important; height:90px !important; }
@media (max-width:1199px) { .adsslot_sd8GuNBX2q{ width:468px !important; height:60px !important; } }
@media (max-width:767px) { .adsslot_sd8GuNBX2q{ width:320px !important; height:50px !important; } }
ADVERTISEMENT
A striking facet of this study involves the obligate role of Porphyromonas gingivalis infection in potentiating macrophage inflammasome responses under hypoxic conditions. This bacterium, long implicated in periodontal disease, has recently garnered attention for its systemic effects, particularly its capacity to modulate immune pathways beyond the oral cavity. The authors provide compelling evidence that P. gingivalis infection primes macrophages to become hyper-responsive to hypoxic stress, thereby exacerbating inflammasome assembly and cytokine release. The intersection of chronic infection and microenvironmental hypoxia creates a vicious cycle that accelerates MS progression.
Utilizing state-of-the-art in vitro and in vivo models, Okano and colleagues meticulously dissected the molecular underpinnings of this process. Their findings reveal that hypoxia-inducible factor 1-alpha (HIF-1α), a key transcriptional regulator activated under low oxygen tensions, orchestrates the upregulation of inflammasome components and inflammatory mediators in infected macrophages. This HIF-1α-dependent pathway underscores a new layer of complexity in immune regulation within the MS microenvironment, highlighting how metabolic stress can converge with pathogenic signals to intensify neuroinflammation.
Further molecular analysis uncovered that P. gingivalis infection enhances the expression of pattern recognition receptors (PRRs) such as NOD-like receptor family pyrin domain containing 3 (NLRP3), which form the core of inflammasome complexes. The dual stimulation by bacterial antigens and hypoxic stress synergistically triggers excessive inflammasome activation, facilitating a chronic pro-inflammatory state deleterious to neuronal integrity. This insight challenges prevailing notions that equate MS solely with autoimmune dysfunction by implicating infectious agents as critical modulators of disease pathology.
The clinical implications of these discoveries are profound. Current MS therapies primarily focus on modulating adaptive immunity. However, this pioneering research suggests that targeting macrophage inflammasome activation, especially under hypoxic conditions influenced by concomitant infections, could herald a new therapeutic frontier. Modulators of HIF-1α signaling or inhibitors of NLRP3 inflammasome assembly may provide potent means to disrupt this detrimental feedback loop, slowing or halting disease progression.
Moreover, understanding the influence of oral microbiota on systemic autoimmune diseases redefines the importance of holistic patient care. The correlation between periodontal health and neurological outcomes underscores the need for interdisciplinary collaboration, integrating dental medicine with neurology and immunology. Preventing or mitigating P. gingivalis infection might reduce the inflammatory burden in MS patients, representing an accessible adjunctive strategy to existing treatments.
The study also emphasizes the nuanced role of the tissue microenvironment in shaping immune cell behavior. It pioneers the concept that hypoxia, commonly observed in inflamed CNS lesions due to impaired vascular supply and increased metabolic demand, is a critical amplifier of neuroimmune responses. The enhanced inflammasome activation in hypoxic macrophages supports the hypothesis that oxygen deprivation is a key pathological feature driving MS symptom exacerbation, potentially accounting for variability in disease severity and progression rates among patients.
In addition to advancing fundamental knowledge, these findings prompt reconsideration of diagnostic and monitoring approaches in MS. Hypoxia-related biomarkers and indicators of inflammasome activation in peripheral immune cells could serve as predictive tools for disease activity or therapeutic efficacy. Such biomarkers would enable personalized medicine strategies, tailoring interventions according to each patient’s inflammatory and metabolic profile.
The research further opens new avenues for exploring the crosstalk between infections and autoimmunity. While the role of P. gingivalis is illuminated here, it raises compelling questions about other microbial species that may exert similar influences on immune dynamics in neuroinflammatory disorders. Characterizing the oral and systemic microbiome in MS patients could reveal broader patterns of microbial involvement and identify novel targets for microbiota-based therapies.
Technologically, the approach combining high-resolution molecular assays, hypoxia chambers, and sophisticated animal models exemplifies the cutting-edge methodologies propelling biomedical research today. The integration of transcriptomic profiling with functional assays enabled the precise delineation of signaling pathways activated in pathological macrophages. This multiplexed strategy ensures that observations extend beyond correlative data, providing mechanistic depth that fosters translational potential.
In sum, this seminal work by Okano et al. heralds a transformative outlook on multiple sclerosis by integrating the roles of cellular metabolism, chronic infection, and immune regulation within the CNS microenvironment. The elucidation of hypoxia-driven inflammasome activation in macrophages infected with Porphyromonas gingivalis charts a complex but actionable landscape where novel interventions may disrupt the cascade leading to neurodegeneration. As the scientific community continues to unravel MS’s multifactorial etiology, such insights underscore the necessity of addressing not only genetic predispositions but also environmental and infectious contributors to disease pathogenesis.
The ramifications of these findings extend beyond MS, potentially informing research into other autoimmune and neurodegenerative conditions where hypoxia and infection intersect. This study exemplifies the power of interdisciplinary inquiry to unlock hidden dimensions of disease and inspire innovative therapeutic paradigms. As such, it stands at the vanguard of neuroimmunology, a beacon guiding future exploration and clinical translation in the relentless quest to alleviate human suffering caused by complex central nervous system disorders.
Subject of Research:
Multiple sclerosis progression mediated by hypoxia-induced inflammasome activation in macrophages infected with Porphyromonas gingivalis
Article Title:
Hypoxia drives progression of multiple sclerosis by enhancing the inflammasome activation in macrophages with Porphyromonas gingivalis infection
Article References:
Okano, T., Ashida, H., Tsukasaki, M. et al. Hypoxia drives progression of multiple sclerosis by enhancing the inflammasome activation in macrophages with Porphyromonas gingivalis infection. Cell Death Discov. 11, 271 (2025). https://doi.org/10.1038/s41420-025-02548-z
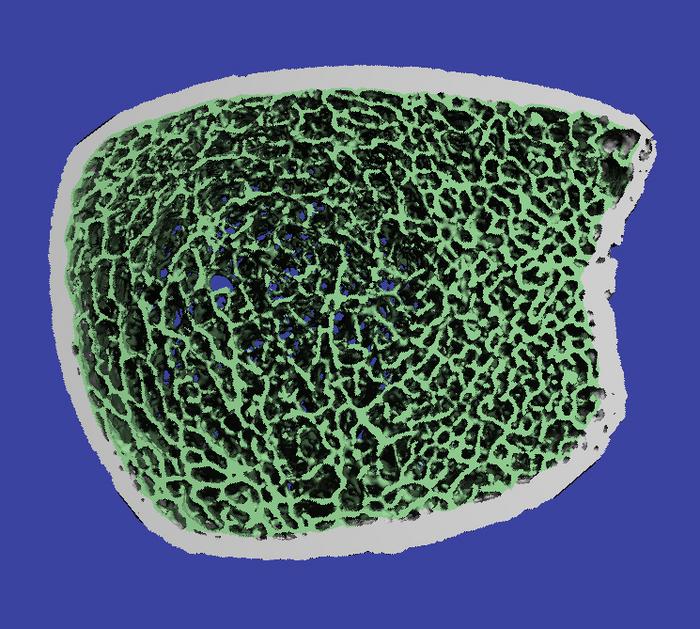
Image Credits: AI Generated
DOI:
https://doi.org/10.1038/s41420-025-02548-z
Tags: central nervous system inflammationchronic autoimmune disease researchchronic infection and MSenvironmental stressors in autoimmune diseaseshypoxia and multiple sclerosisimmune response modulation in MSlow oxygen levels and immune dysfunctionmacrophage inflammasome activationmacrophage plasticity in immune responseneurodegenerative disease progression mechanismsPorphyromonas gingivalis and neuroinflammationtherapeutic targets for multiple sclerosis
What's Your Reaction?