Common chemotherapy drugs don’t work like doctors thought, with big implications for drug discovery
A new study from the University of Wisconsin–Madison suggests that chemotherapy may not be reaching its full potential, in part because researchers and doctors have long misunderstood how some of the most common cancer drugs actually ward off tumors. Credit: Beth Weaver, University of Wisconsin–Madison A new study from the University of Wisconsin–Madison suggests that […]

A new study from the University of Wisconsin–Madison suggests that chemotherapy may not be reaching its full potential, in part because researchers and doctors have long misunderstood how some of the most common cancer drugs actually ward off tumors.

Credit: Beth Weaver, University of Wisconsin–Madison
A new study from the University of Wisconsin–Madison suggests that chemotherapy may not be reaching its full potential, in part because researchers and doctors have long misunderstood how some of the most common cancer drugs actually ward off tumors.
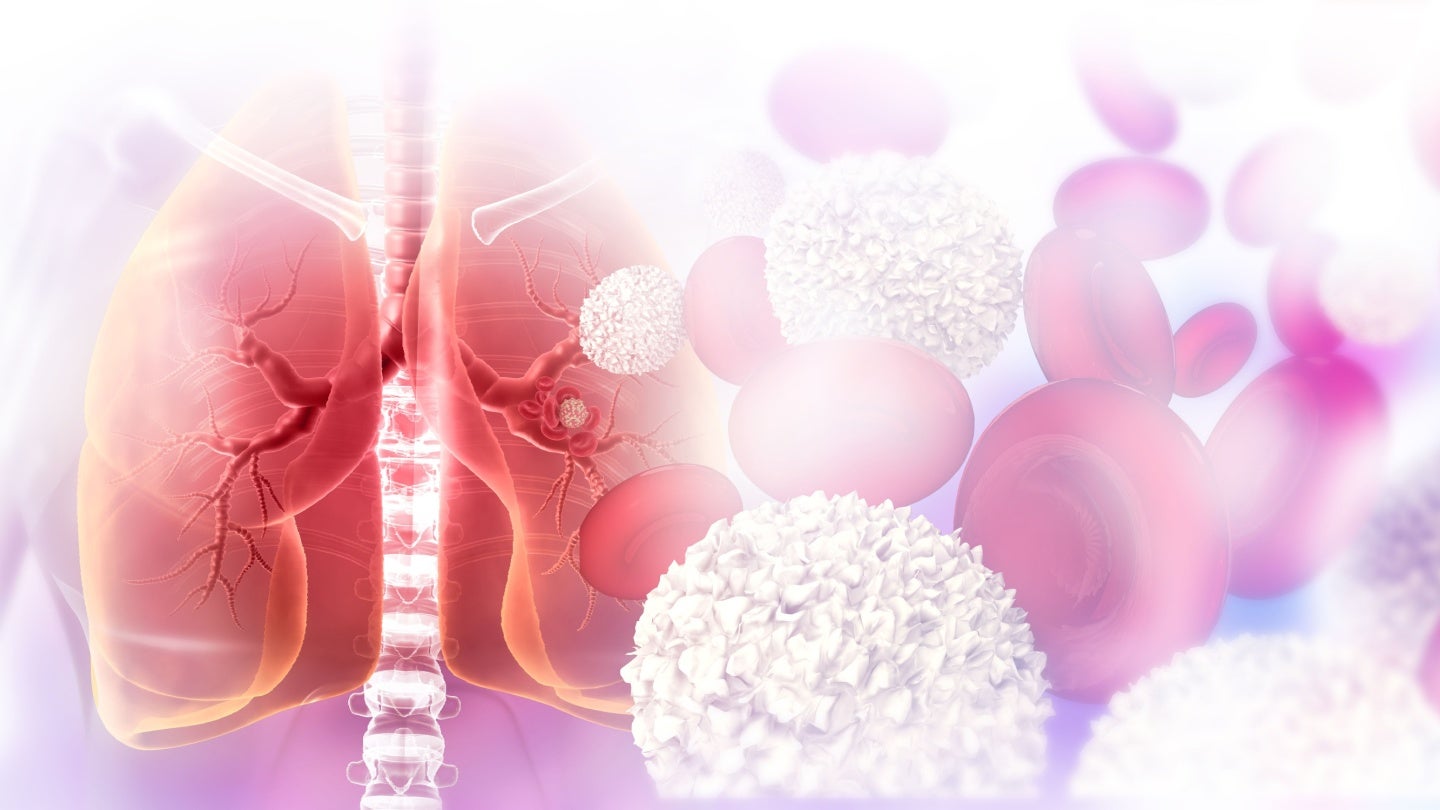
For decades, researchers have believed that a class of drugs called microtubule poisons treat cancerous tumors by halting mitosis, or the division of cells. Now, a team of UW–Madison scientists has found that in patients, microtubule poisons don’t actually stop cancer cells from dividing. Instead, these drugs alter mitosis — sometimes enough to cause new cancer cells to die and the disease to regress.
Cancers grow and spread because cancerous cells divide and multiply indefinitely, unlike normal cells which are limited in the number of times they can split into new cells. The assumption that microtubule poisons stop cancer cells from dividing is based on lab studies demonstrating just that.
The new study was led by Beth Weaver, a professor in the departments of oncology and cell and regenerative biology, in collaboration with Mark Burkard in the departments of oncology and medicine. Published Oct. 26 in the journal PLOS Biology and supported in part by the National Institutes of Health, the study broadens previous findings the group made about a specific microtubule poison called paclitaxel. Sometimes prescribed under the brand name Taxol, paclitaxel is used to treat common malignancies including those originating in the ovaries and lungs.
“This was sort of mind-blowing,” Weaver says about the previous research. “For decades, we all thought that the way paclitaxel works in patient tumors is by arresting them in mitosis. This is what I was taught as a graduate student. We all ‘knew’ this. In cells in a dish, labs all over the world have shown this. The problem was we were all using it at concentrations higher than those that actually get into the tumor.”
Weaver and her colleagues wanted to know if other microtubule poisons work the same way as paclitaxel — not by stopping mitosis but by messing it up.
The question has significant implications for scientists searching for new cancer treatments. That’s because drug discovery efforts often hinge on identifying, reproducing and improving upon the mechanisms believed to be responsible for a compound’s therapeutic effect.
While microtubule poisons are no panacea, they are effective for many patients, and researchers have long sought to develop other therapies that mimic what they believe the drugs do. These efforts are ongoing even though past attempts to identify new compounds that treat cancer by stopping cell division have reached frustrating dead ends.
“There’s still a lot of the scientific community that’s investigating mitotic arrest as a mechanism to kill tumors,” Weaver says. “We wanted to know — does that matter for patients?”
With Burkard, the team studied tumor samples taken from breast cancer patients who received standard anti-microtubule chemotherapy at the UW Carbone Cancer Center.
They measured how much of the drugs made it into the tumors and studied how the tumor cells responded. They found that while the cells continued to divide after being exposed to the drug, they did so abnormally. This abnormal division can lead to tumor cell death.
Normally, a cell’s chromosomes are duplicated before the two identical sets migrate to opposite ends of the cell mitosis in a process called chromosomal segregation. One set of chromosomes is sorted into each of two new cells.
This migration occurs because the chromosomes are attached to a cellular machine known as the mitotic spindle. Spindles are made from cellular building blocks called microtubules. Normal spindles have two ends, known as spindle poles.
Weaver and her colleagues found that paclitaxel and other microtubule poisons cause abnormalities that lead cells to form three, four or sometimes five poles during mitosis even as they continue to make just one copy of chromosomes. These poles then attract the two complete sets of chromosomes in more than two directions, scrambling the genome.
“So, after mitosis you have daughter cells that are no longer genetically identical and have lost chromosomes,” Weaver says. “We calculated that if a cell loses at least 20% of its DNA content, it is very likely going to die.”
These findings reveal the likely reason why microtubule poisons are effective for many patients. Importantly, they also help explain why attempts to find new chemo drugs based solely on stopping mitosis have been so disappointing, Weaver says.
“We’ve been barking up the wrong tree,” she says. “We need to refocus our efforts on screwing up mitosis — on making chromosomal segregation worse.”
This research was supported in part by the National Institutes of Health (P30 CA014520; R01CA234904; T32 GM008688; T32 CA009135; F31CA254247; T32 GM141013).
Journal
PLoS Biology
DOI
10.1371/journal.pbio.3002339
Article Title
Diverse microtubule-targeted anticancer agents kill cells by inducing chromosome missegregation on multipolar spindles
Article Publication Date
26-Oct-2023
What's Your Reaction?