Breakthroughs in Science Unlock Treatments for the Most Challenging Bladder Cancers
In a groundbreaking study poised to reshape the therapeutic landscape of bladder cancer, researchers at the University of California, San Francisco (UCSF) have unveiled a novel approach to identify and target a notoriously elusive subtype of the disease known as histologic variant (HV) bladder cancer. This form of bladder tumor, which accounts for nearly 25% […]


In a groundbreaking study poised to reshape the therapeutic landscape of bladder cancer, researchers at the University of California, San Francisco (UCSF) have unveiled a novel approach to identify and target a notoriously elusive subtype of the disease known as histologic variant (HV) bladder cancer. This form of bladder tumor, which accounts for nearly 25% of all bladder cancer cases yet remains largely excluded from clinical trials, has confounded oncologists due to its heterogeneity and resistance to conventional treatments.
Unlike typical bladder cancers that exhibit predictable histological features and respond to established therapeutic regimens, HV bladder cancers display a bewildering array of morphological variations under microscopic examination. These tumors often evade standard chemotherapy and immunotherapy, leaving radical surgery as the primary, albeit insufficient, curative option. The recurrence rate remains alarmingly high, underscoring an urgent need for innovative, targeted treatment modalities.
The UCSF team employed an advanced single-cell sequencing platform developed within their lab, allowing unprecedented resolution insight into the genetic and molecular underpinnings of these diverse tumors. By analyzing gene expression profiles at the individual tumor cell level, they discerned a unique molecular signature shared across HV subtypes. Most strikingly, the presence of the carbohydrate antigen 125 (CA125), a marker conventionally associated with ovarian malignancies, was identified on the surface of HV tumor cells but conspicuously absent in conventional bladder cancers.
.adsslot_8H3bF2RwNU{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_8H3bF2RwNU{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_8H3bF2RwNU{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
This unexpected discovery of CA125 expression in bladder tumors challenged existing paradigms and opened new therapeutic avenues. Guided by this insight, the researchers further characterized HV tumors and uncovered the consistent expression of TM4SF1, a transmembrane protein implicated in tumor progression and metastasis. This protein emerged as a promising target for immunotherapeutic intervention, spurring the development of chimeric antigen receptor T-cell (CAR-T) therapy engineered specifically to seek and eradicate TM4SF1-expressing tumor cells.
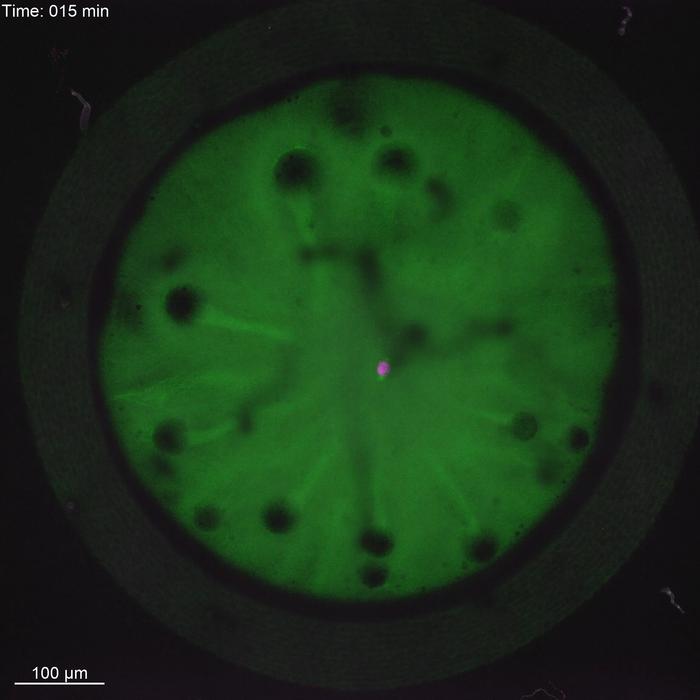
In preclinical models, CAR-T cells designed to recognize TM4SF1 demonstrated remarkable efficacy, homing to bladder tumors in mice and eliminating malignant cells with precision. These results mark a pivotal advancement, offering compelling evidence that immunotherapy tailored to HV bladder cancer’s unique molecular landscape might overcome the traditional barriers posed by tumor heterogeneity.
Crucial to this breakthrough was the integration of cutting-edge genomic technologies with translational oncology expertise. By leveraging single-cell RNA sequencing, the UCSF researchers deciphered the complex tumor microenvironment and pinpointed molecular vulnerabilities previously concealed within the diverse cellular tapestry of HV bladder cancers. This technological synergy accelerated the translation from tumor characterization to therapeutic innovation within a remarkably condensed timeframe.
As Dr. Sima Porten, co-senior author and associate professor of urology at UCSF, delineated, the conventional clinical approach to HV bladder tumors has been constrained by their variability and the consequent challenges in standardizing treatment strategies. The UCSF team’s findings herald a new epoch where individualized molecular markers like CA125 and TM4SF1 can serve as linchpins for precision medicine, enabling personalized immunotherapeutic interventions.
The implications for patient care are profound. Patients battling HV bladder cancer typically face a grim prognosis due to the paucity of effective systemic therapies. The potential to harness CAR-T cell therapy against TM4SF1-expressing tumors delivers hope for durable responses, possibly transforming an often-fatal diagnosis into a manageable condition. Moreover, the ability to stratify patients based on tumor molecular profiles promises to refine clinical trial designs, fostering inclusive studies that encompass this previously neglected patient cohort.
One of the study’s notable aspects is the multidisciplinary collaboration spanning urology, oncology, genomics, and immunotherapy. The amalgamation of expertise catalyzed the comprehensive analysis of tumor biology and therapeutic engineering, exemplified by the contributions of leading scientists such as Dr. Franklin Huang, who emphasized the translational impact of their single-cell sequencing platform in fast-tracking the identification of actionable targets.
Funding from esteemed entities including the National Institutes of Health (NIH), the Chan-Zuckerberg Biohub, and dedicated urology foundations was instrumental in sustaining this multifaceted research endeavor. Such support underscores the vital importance of fostering innovative cancer research infrastructure capable of bridging fundamental science and clinical application.
While the preclinical success of TM4SF1-targeted CAR-T therapy is promising, the path toward clinical implementation warrants meticulous evaluation. Future studies will need to address therapeutic safety, efficacy in human subjects, potential off-target effects, and the durability of anti-tumor responses. Nonetheless, this groundwork lays a robust foundation for advancing clinical trials tailored to HV bladder cancer patients.
Furthermore, this research ignites a broader discourse on the necessity of integrating high-resolution molecular profiling technologies in oncology. The heterogeneous nature of many cancers demands approaches that begin with understanding the tumor’s cellular heterogeneity at the single-cell level, which can uncover concealed therapeutic targets and resistance mechanisms.
In summation, the UCSF discovery epitomizes how precision medicine, empowered by sophisticated genomic tools and immunotherapy innovation, can redefine treatment paradigms for challenging cancers. The identification of CA125 and TM4SF1 as biomarkers and immunotherapeutic targets in HV bladder tumors inaugurates a hopeful chapter for patients with limited options and inspires a strategic recalibration of future bladder cancer clinical research.
Subject of Research: Histologic variant bladder cancer and targeted immunotherapy development
Article Title: Unavailable
News Publication Date: June 17 (Year not specified)
Web References: Article published in Nature Communications
References: Funded by Chan-Zuckerberg Biohub, UCSF Department of Medicine, NIH (TL1DK139565, U2CDK133488), Urology Care Foundation, California Urology Foundation
Keywords: Cancer, Chimeric antigen receptor therapy, Tumor tissue, Ovarian cancer, Urology, Proteins
Tags: advancements in cancer therapeuticsbladder cancer breakthroughsCA125 as a cancer markerchallenges in bladder cancer treatmenthistologic variant bladder cancerinnovative therapies for resistant cancersmolecular profiling of tumorsrecurrence rates in bladder cancersingle-cell sequencing in oncologytargeted treatments for bladder cancerUCSF cancer researchunderstanding tumor heterogeneity
What's Your Reaction?