Breakthrough Study Advances Personalized Immunotherapy Approaches for Pediatric Cancers
Researchers at Karolinska Institutet, in conjunction with the Astrid Lindgren Children’s Hospital in Sweden, have undertaken a pivotal study focused on the immune responses of children encountering different forms of cancer, with a particular emphasis on age-related variances. The research, recently published in the esteemed journal Cell, reveals profound differences in immune reactions between children […]


Researchers at Karolinska Institutet, in conjunction with the Astrid Lindgren Children’s Hospital in Sweden, have undertaken a pivotal study focused on the immune responses of children encountering different forms of cancer, with a particular emphasis on age-related variances. The research, recently published in the esteemed journal Cell, reveals profound differences in immune reactions between children and adults battling cancer, a discovery that harbors the potential to revolutionize treatment paradigms for pediatric oncology. Understanding how a child’s immune system interacts with different cancers could lead to markedly more tailored and effective therapeutic options.
At the forefront of this groundbreaking research, Professor Petter Brodin—a noted expert in pediatric immunology—emphasizes the necessity of comprehending the unique immune dynamics at play in the context of childhood cancer. He points out that the activation pathways of the immune system, critical for combating tumors, show significant divergence between young patients and their adult counterparts. This distinction underlines the imperative for more in-depth investigations into the regulatory mechanisms governing immune responses in children, who are confronted with various malignancies. The findings of this study promise to illuminate new pathways for improved treatment strategies tailored specifically for the pediatric population.
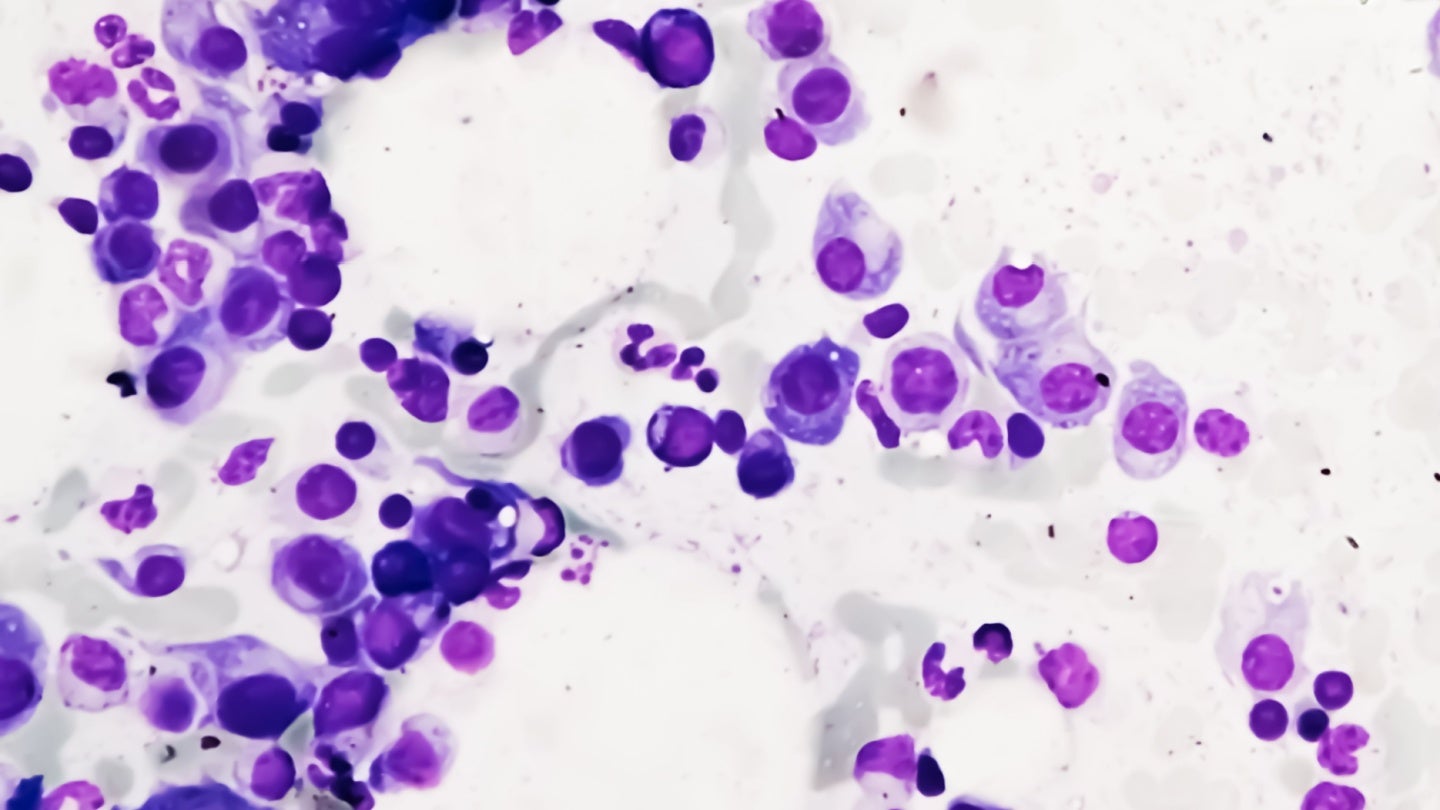
The study encompassed a cohort of 191 children aged 0 to 18, all of whom had been diagnosed with various types of solid tumors at the Astrid Lindgren Children’s Hospital over six years, from 2018 to 2024. By meticulously analyzing tumor tissues and blood samples, the researchers endeavored to pinpoint genetic mutations present in the tumors, while also assessing which immune-related genes were active or dormant. This comprehensive genetic insight is a vital component in creating a detailed portrait of how a child’s immune system responds to cancer.
Professor Brodin elaborates that the prevailing principles of precision medicine in oncology have primarily concentrated on the characteristics of the tumors themselves. However, this study marks a profound shift by incorporating the role of the immune system into the equation. Characterizing immune profiles introduces a vital new perspective, one that is likely to shape and refine the future of cancer therapies aimed at children. This fresh approach could serve as a foundational element in devising treatments that are not only more effective but also customized to individual patient profiles.
Intriguingly, the research outcomes indicate that the immune systems of children and adults display disparate reactions to cancerous growths. The study highlighted that tumors in children tend to elicit a less inflammatory response and possess fewer mutations, leading to a scenario where these tumors may appear more insidious and less recognizable to the developing immune system. Consequently, this results in a less vigorous attack from the immune cells tasked with eliminating these malignant cells. However, large inter-individual variations were also noted, reinforcing the necessity of a precision medicine framework that tailors treatment approaches to the unique immune landscape of each pediatric patient.
Furthermore, the implications of the findings extend into the domain of immunotherapy, a treatment approach that has gained traction among adult cancer patients. The study offers significant insights into why traditional immunotherapeutic strategies, such as checkpoint inhibitors—which work by enhancing immune cell efficacy against tumors—might not yield the same benefits in children. Professor Brodin argues that this therapeutic modality relies on an armament of immune cells pre-activated against the tumor, yet many children demonstrate a lack of this immune readiness. Such findings underscore a pressing need for new forms of immunotherapy that better engage and stimulate the immune response in children from the onset of treatment.
Throughout the study, the researchers took a longitudinal approach, diligently monitoring the immune responses of some child patients throughout their treatment regimen. This innovative tracking allowed for the assessment of dynamic changes, particularly in the populations of killer T cells—key effector cells involved in the destruction of tumor cells. The ability to observe and measure these shifts in immune function holds immense promise for real-world clinical applications, potentially enabling healthcare practitioners to adapt treatment plans on an individual basis. Such customizations could substantially enhance therapeutic effectiveness, providing a much-needed complement to existing genetic analyses performed in routine pediatric oncology care.
The collaborative effort behind this study also warrants mention. Led by Professor Brodin and his colleague Linda Ljungblad, an oncology resident, the study represents a synergistic partnership with the pediatric oncology clinic at the Astrid Lindgren Children’s Hospital. Such interdisciplinary collaborations are crucial in fostering advancements in pediatric cancer research, as they combine clinical insights with cutting-edge scientific inquiry. Additionally, the financial backing received from notable organizations including the Swedish Cancer Society and the Swedish Childhood Cancer Foundation highlights the growing interest and investment in understanding and addressing pediatric cancers.
While this groundbreaking research lays a foundation for future advancements, it also raises a multitude of questions regarding the complex interplay of genetics and the immune system in the pediatric setting. It prompts us to consider the broader implications for childhood cancer treatment, potentially fostering a new wave of investigational therapies that pivot away from adult-centric paradigms. Such shifts could transform how we approach not only cancer care but also the underlying biology of tumors in children and the accompanying immune responses.
As further investigations are conducted on a larger scale, the promise of this research extends beyond the initial findings. The ability to merge immune profiling with genetic data could catalyze a new standard in how healthcare providers assess and treat childhood cancer, tailoring therapies that account for the unique immunological landscape of each child. This research is a clarion call to the scientific community, urging a reevaluation of current strategies in pediatric oncology. It lays the groundwork for future studies targeting the underlying mechanisms that govern immune interactions with tumors, ensuring that children receive the most beneficial care possible.
Ultimately, the hopes from this research extend into tangible clinical outcomes for young cancer patients. With an inspiring momentum towards innovation in pediatric cancer care, the work being done at Karolinska Institutet and the Astrid Lindgren Children’s Hospital illuminates pathways toward a future where cancer therapies are as individualized and nuanced as the patients they aim to heal. The commitment to understanding pediatric immune responses is crucial for breaking new ground in the fight against cancer, equipping the next generation of patients with the best chance for survival and recovery.
Subject of Research: The immune system’s response to childhood cancer
Article Title: Systems-level immunomonitoring in children with solid tumors to enable precision medicine
News Publication Date: 20-Jan-2025
Web References: https://doi.org/10.1016/j.cell.2024.12.014
References: Not applicable
Image Credits: Not applicable
Keywords: Cancer research, Children, Immune response, Cancer immunotherapy, Clinical research, Research on children, Solid tumors, Genetic analysis, Drug therapy, Immunology, Oncology, Pediatrics, Immune system
What's Your Reaction?