Brain Metastases Re-Resection: Outcomes Revealed
In the evolving landscape of neuro-oncology, brain metastases pose a formidable challenge, often impacting patient survival and quality of life. Recent advances in microsurgical techniques and adjuvant therapies have improved outcomes for many, yet recurrence remains a significant hurdle. Addressing this critical issue, a new institutional cohort study published in BMC Cancer illuminates the landscape […]


In the evolving landscape of neuro-oncology, brain metastases pose a formidable challenge, often impacting patient survival and quality of life. Recent advances in microsurgical techniques and adjuvant therapies have improved outcomes for many, yet recurrence remains a significant hurdle. Addressing this critical issue, a new institutional cohort study published in BMC Cancer illuminates the landscape of re-resection as a viable treatment strategy for recurrent brain metastases, offering fresh insight into its clinical outcomes and therapeutic potential.
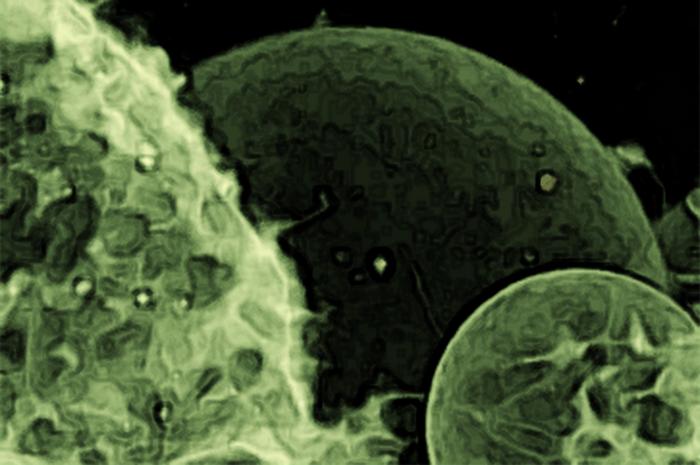
Brain metastases, secondary tumors originating from cancers such as non-small cell lung cancer (NSCLC), breast cancer, and melanoma, frequently mandatorily require aggressive surgical intervention followed by radiation therapy. The standard initial approach typically involves microsurgical removal, which aims to debulk tumor burden and alleviate neurological symptoms, succeeded by focused radiation to eradicate residual malignant cells. Despite these interventions, however, a considerable proportion of patients experience intracranial recurrence, either locally at the original site or distantly within the brain, complicating treatment pathways.
The study, a single-center retrospective analysis, evaluated 60 patients who underwent a secondary surgical resection after an initial procedure coupled with radiotherapy. Notably, this research sheds light on the nuanced considerations that intervene in decisions surrounding re-resection—particularly in an era increasingly defined by precision oncology. Local recurrences represented approximately two-thirds of cases (68.3%), while the remaining third (31.7%) comprised distant recurrences, emphasizing the heterogeneity of metastatic progression within cerebral compartments.
.adsslot_tquNpP1bzA{width:728px !important;height:90px !important;}
@media(max-width:1199px){ .adsslot_tquNpP1bzA{width:468px !important;height:60px !important;}
}
@media(max-width:767px){ .adsslot_tquNpP1bzA{width:320px !important;height:50px !important;}
}
ADVERTISEMENT
A key revelation of the investigation lies in the survival metrics post-re-resection. Median intracranial progression-free survival was recorded at 7.7 months, highlighting the temporary but meaningful disease control achievable with surgical intervention. More strikingly, the median overall survival extended to 30.8 months, signaling a potential for prolonged life expectancy in select patients undergoing this aggressive repeat surgical approach. Such data challenge the traditional skepticism surrounding second surgeries in recurrent brain metastasis.
The study foregrounds non-small cell lung cancer (NSCLC) as the predominant primary malignancy in the cohort, aligning with broader epidemiological trends that underscore NSCLC’s proclivity for cerebral dissemination. Treatment after initial resection varied widely, ranging from radiation monotherapy to combinations with chemotherapy, targeted agents, or immunotherapies, reflecting the multidimensional and personalized nature of contemporary neuro-oncologic care. Cavity irradiation was employed in the majority of cases, affirming its role in sterilizing postoperative zones vulnerable to microscopic residual disease.
Post-re-resection therapeutic strategies demonstrated marked heterogeneity, with some patients receiving solely best supportive care, while others underwent radiation, systemic therapies, or their combinations. This variation underscores the complexity in defining standardized protocols, emphasizing the need for individualized treatment paradigms contingent upon patient performance status, tumor characteristics, and prior interventions.
Crucially, the research identifies four independent prognostic factors correlated with survival outcomes: histology other than breast cancer, pre-re-resection tumor volumes exceeding 9 mL, compromised functional capacity as measured by a Karnofsky Performance Status (KPS) of 60% or below, and the presence of viable tumor cells at the time of re-resection. These parameters provide invaluable guidance for clinicians in stratifying patients, anticipating surgical benefit, and tailoring follow-up treatments.
The resection of brain metastases recurrent at both local and distant sites is portrayed as not merely feasible but strategically advantageous in carefully selected patients. This challenges the prevailing paradigm that recurrent intracranial disease is uniformly associated with poor prognosis and limited therapeutic options. Instead, it advocates for a reassessment of surgical eligibility criteria incorporating tumor biology, volumetric analysis, and functional scales.
From a technical perspective, the study highlights the advancements in microsurgical precision and perioperative care that mitigate risks commonly associated with brain surgery, including neurological deficits and infection. Coupling these advances with sophisticated imaging techniques enables surgeons to delineate pathological tissue with increasingly refined margins, which may contribute to enhanced local control following re-resection.
Equally pivotal is the emphasis on multidisciplinary management. The integration of neurosurgery, radiation oncology, medical oncology, and supportive care teams ensures a comprehensive approach to recurrent brain metastases, optimizing not only survival but also quality of life. Interdisciplinary collaboration also supports nuanced decision-making, balancing the benefits and potential morbidities of repeat surgery against other therapeutic modalities.
While the study is retrospective and single-center, limiting wider immediate generalizability, it charts a critical course for future research. Prospective studies with larger cohorts and incorporation of molecular markers could further refine patient selection, optimize perioperative protocols, and elucidate the synergistic effects of combined systemic and local therapies following re-resection.
This investigation ultimately carries profound implications for the rapidly expanding population of cancer survivors suffering intracranial disease recurrence. As systemic cancer therapies extend systemic control, the brain increasingly emerges as a sanctuary site for metastases, necessitating refined local treatment strategies such as re-resection. The data advocate for integrating surgical options more robustly into salvage treatment algorithms, reshaping therapeutic horizons.
In conclusion, this breakthrough research advocates for reconsidering re-resection of brain metastases as a vital component of multidisciplinary oncology care. By delineating clinical parameters predictive of benefit and survival, it empowers physicians with evidence-based criteria to select candidates most likely to gain from aggressive surgical salvage. As the oncology community grapples with the complexities of recurrent brain metastases, these findings illuminate a pathway forward, blending surgical innovation with personalized medicine to enhance patient outcomes.
The findings also underscore the vital necessity of ongoing clinical trials and real-world studies to delineate optimal sequencing of surgery, radiotherapy, and systemic treatments. Harnessing emerging targeted and immune-based therapies in tandem with surgical interventions promises further improvements in controlling intracranial disease.
As brain metastases continue to complicate cancer care worldwide, this study reinvigorates hope by establishing re-resection as more than a last resort—potentially a standard of care in select circumstances. The neuro-oncology field awaits subsequent research to validate and expand upon these promising initial insights, heralding a new era of refined and effective management for recurrent brain metastases.
Subject of Research: Clinical and treatment outcomes following re-resection of recurrent brain metastases in cancer patients.
Article Title: Re-resection of brain metastases – outcomes of an institutional cohort study and literature review
Article References:
Wasilewski, D., Shaked, Z., Fuchs, A. et al. Re-resection of brain metastases – outcomes of an institutional cohort study and literature review. BMC Cancer 25, 973 (2025). https://doi.org/10.1186/s12885-025-13677-0
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-13677-0
Tags: adjuvant therapies for brain metastasesbrain metastases treatment outcomesinstitutional cohort study on brain tumorsintracranial tumor recurrence challengesmicrosurgical techniques for brain tumorsneuro-oncology advancementsnon-small cell lung cancer brain metastasespatient survival with brain metastasesprecision oncology in brain metastasesrecurrent brain tumor re-resectionsecondary surgical resection in cancertherapeutic potential of re-resection
What's Your Reaction?