Autologous Stem Cell Transplants in ALL Remission
Autologous Stem Cell Transplantation Emerges as a Promising Approach for Philadelphia-Negative Acute Lymphoblastic Leukemia in Adults Philadelphia chromosome-negative acute lymphoblastic leukemia (Ph-ALL) represents a challenging hematologic malignancy that demands innovative therapeutic strategies for improved patient outcomes. A groundbreaking retrospective study, recently published in BMC Cancer, sheds new light on the role of autologous hematopoietic stem […]


Autologous Stem Cell Transplantation Emerges as a Promising Approach for Philadelphia-Negative Acute Lymphoblastic Leukemia in Adults
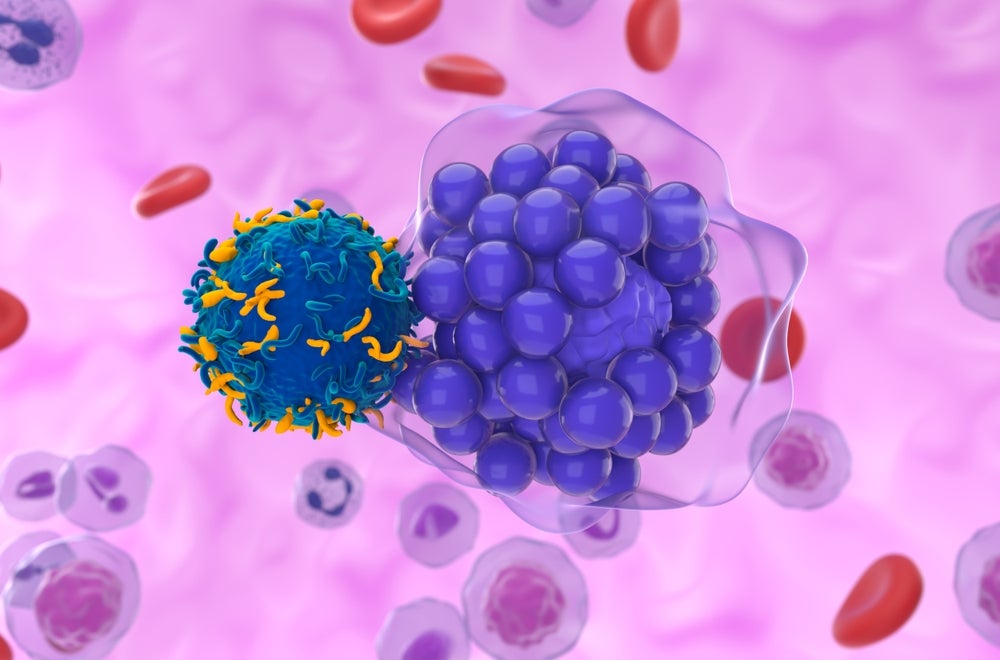
Philadelphia chromosome-negative acute lymphoblastic leukemia (Ph-ALL) represents a challenging hematologic malignancy that demands innovative therapeutic strategies for improved patient outcomes. A groundbreaking retrospective study, recently published in BMC Cancer, sheds new light on the role of autologous hematopoietic stem cell transplantation (AHSCT) for adults with Ph-ALL who have achieved first complete remission. This extensive analysis, conducted by the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation (EBMT), analyzes data spanning over two decades and provides compelling evidence on survival benefits and prognostic factors influencing transplantation success.
Historically, treatment options for adult Ph-ALL have been limited and often hampered by the aggressive nature of the disease and treatment-related toxicities. Allogeneic stem cell transplantation has been the gold standard for eligible patients, but this procedure carries significant risks such as graft-versus-host disease and high treatment-related mortality. Against this backdrop, the potential of autologous transplantation, wherein the patient’s own stem cells are utilized, has been intensely debated. The current study aims to clarify these uncertainties by analyzing outcomes in a large patient cohort.
The investigators compiled data from 700 adults who underwent AHSCT while in first complete remission between 1999 and 2020. This cohort, with a median age of approximately 32 years and predominantly male representation, included a significant representation of two main immunophenotypic subtypes: B-cell precursor ALL (BCP-ALL) constituting 35%, and T-cell precursor ALL (TCP-ALL) accounting for 65%. Importantly, for a subset of 190 patients, minimal residual disease (MRD) status was available, with a remarkable 88% deemed MRD-negative prior to transplantation, underscoring the depth of remission in these cases.
Outcome analyses reveal that AHSCT offers a relatively favorable safety profile and meaningful survival advantages. At the two-year mark, overall survival (OS) was estimated at 67%, while leukemia-free survival (LFS) stood at 56%. These findings mark an encouraging sign, especially considering the intensity and refractory potential of Ph-ALL. Disease relapse remains a key challenge, with a reported incidence of 39%. However, non-relapse mortality (NRM) was notably low at 5%, indicating minimal transplant-related toxicity in this setting.
Intriguingly, patient outcomes differed significantly according to ALL immunophenotype. Those diagnosed with TCP-ALL demonstrated a lower relapse incidence (41% vs. 56%) in comparison to BCP-ALL patients. This translated into higher five-year leukemia-free survival (52% vs. 38%) and overall survival rates (58% vs. 45%) for TCP-ALL individuals. These differences emphasize the heterogeneity within Ph-ALL and suggest distinct biological behavior and treatment responsiveness between the subtypes.
The study’s rigorous multivariate analysis further identified prognostic factors impacting transplantation outcomes. A diagnosis of TCP-ALL and a longer interval from initial diagnosis to transplantation were both independently linked to reduced relapse risk, better leukemia-free survival, and improved overall survival. Conversely, increasing patient age emerged as a significant adverse factor, correlating with higher non-relapse mortality and inferior survival metrics. These findings underscore the critical importance of individualized treatment planning based on disease biology and patient demographics.
From a mechanistic standpoint, autologous transplantation offers the advantage of lower toxicity while still enabling dose intensification after induction chemotherapy. Utilizing a patient’s own hematopoietic stem cells minimizes immunological complications yet allows for aggressive myeloablative regimens aimed at eradicating residual leukemic clones. The data presented validate this therapeutic rationale in a real-world context, with encouraging survival outcomes in a challenging patient population.
Though retrospective in nature, the study provides one of the most comprehensive assessments of AHSCT in adult Ph-ALL to date. It highlights the pressing need for prospective clinical trials to confirm these observations and optimize the role of autologous transplantation within contemporary treatment algorithms. Future investigations focusing on integrating MRD monitoring, novel targeted agents, and refined conditioning regimens hold promise to further enhance patient prognosis.
Furthermore, the findings prompt a reassessment of therapeutic strategies for TCP-ALL, where autologous transplantation seems particularly advantageous. Given the paucity of tailored therapies for this subset, AHSCT may represent a timely intervention that balances efficacy and tolerability, pending causal confirmation through clinical trials. This nuanced appreciation of disease subtypes could usher in precision medicine approaches in acute leukemia management.
The generally low non-relapse mortality rates found in this population affirm the feasibility of AHSCT as a relatively safe intensification modality, especially in younger, well-selected patients. The identification of age as a limiting factor serves as a cautionary note, emphasizing meticulous patient selection and supportive care optimization to mitigate risks in older individuals undergoing transplantation.
In summary, this large-scale EBMT study resurrects autologous stem cell transplantation as a viable therapeutic maneuver in adult Ph-ALL, especially in patients exhibiting favorable biological features like TCP-ALL immunophenotype and low MRD. The data challenge previous skepticism towards AHSCT in this context and pave the way for its reintegration into treatment schemes alongside novel systemic therapies.
This work marks a significant milestone that could influence clinical guidelines and inspire future international collaborations striving to refine transplant strategies in hematologic malignancies. Grounded on robust survival data and risk stratification, autologous transplantation now stands out as a promising, safe, and potentially curative option in the adult Ph-ALL therapeutic arsenal.
Ultimately, with continued research and validation, AHSCT may serve as a critical pivot in personalizing leukemia care, optimizing long-term remission, reducing treatment-related morbidity, and improving quality of life for adults facing this formidable disease.
Subject of Research: Autologous hematopoietic stem cell transplantation outcomes in adults with Philadelphia chromosome-negative acute lymphoblastic leukemia in first complete remission.
Article Title: Autologous stem cell transplantation for adults with Philadelphia-negative acute lymphoblastic leukemia in first complete remission. A study by the Acute Leukemia Working Party of the EBMT
Article References:
Swoboda, R., Labopin, M., Giebel, S. et al. Autologous stem cell transplantation for adults with Philadelphia-negative acute lymphoblastic leukemia in first complete remission. A study by the Acute Leukemia Working Party of the EBMT. BMC Cancer 25, 787 (2025). https://doi.org/10.1186/s12885-025-14126-8
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14126-8
Tags: adult leukemia treatment optionsallogeneic vs autologous stem cell transplantautologous stem cell transplantationBMC Cancer studycomplete remission in Ph-ALL patientsEBMT research on leukemiahematopoietic stem cell transplantationpatient outcomes in leukemiaPhiladelphia-negative acute lymphoblastic leukemiaprognostic factors in stem cell transplantsurvival benefits of AHSCTtreatment-related toxicities in leukemia
What's Your Reaction?