A study by UPF and BCNatal opens the door to designing therapies to improve lung development in growth-restricted fetuses
If during a pregnancy a fetus grows below normal thresholds, at each week of gestation there is an increased risk that some of its organs may not develop properly, which can adversely affect the baby’s health after birth. The life-long effects of restricted fetal growth on brain and cardiovascular development have been the subject of […]
If during a pregnancy a fetus grows below normal thresholds, at each week of gestation there is an increased risk that some of its organs may not develop properly, which can adversely affect the baby’s health after birth. The life-long effects of restricted fetal growth on brain and cardiovascular development have been the subject of much research, but there is a lack of scientific evidence on its impact on the lungs.
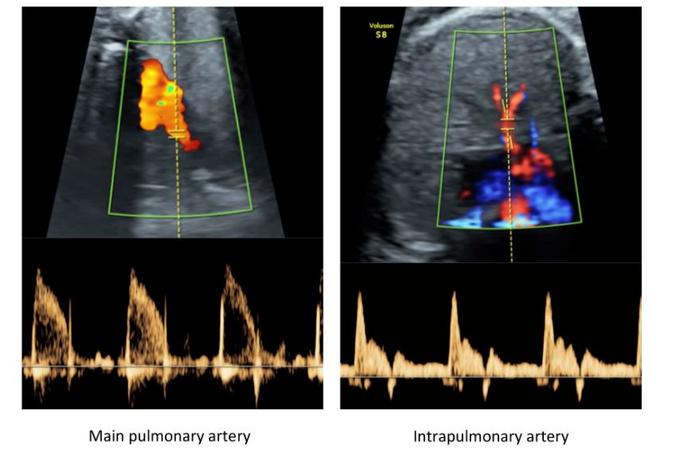
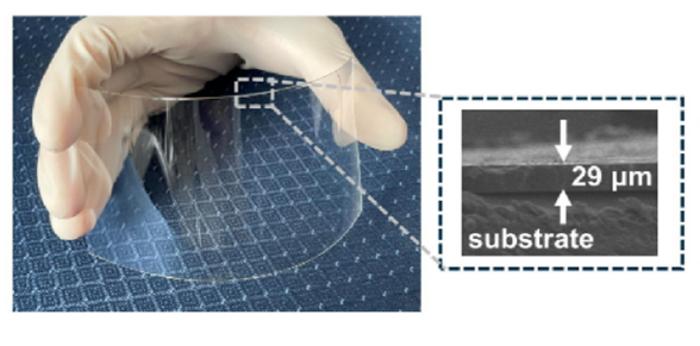
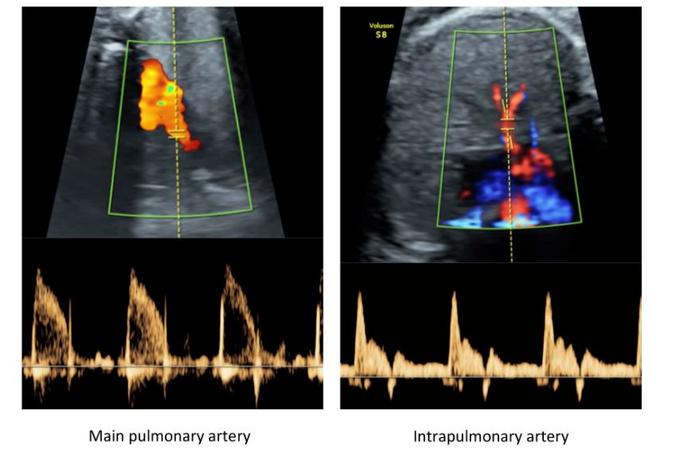
Credit: Vellvé, K., Garcia-Canadilla, P., Nogueira, M. et al.
If during a pregnancy a fetus grows below normal thresholds, at each week of gestation there is an increased risk that some of its organs may not develop properly, which can adversely affect the baby’s health after birth. The life-long effects of restricted fetal growth on brain and cardiovascular development have been the subject of much research, but there is a lack of scientific evidence on its impact on the lungs.
This is the focus of research led jointly by the BCNatal Fetal Medicine Research Center (Hospital Clínic Barcelona and Hospital Sant Joan de Déu) and UPF, which has led to detecting differences in the development of the lungs of growth-restricted and normal fetuses, in terms of their vascular resistance. The researchers studied this by measuring blood velocity in the fetus and analysing this with the support of artificial intelligence techniques and computer models.
The results of the study, recently reported in an article in the journal Scientific Reports (Nature), open the door to designing therapies to improve the lung development of fetuses with below-normal growth levels and prevent respiratory health problems, which could extend beyond infancy and into adolescence and adulthood.
The principal researchers of the study are Fátima Crispi, a researcher at BCNatal and Clínic-IDIBAPS in the Fetal and Perinatal Medicine group, and Bart Bijnens (ICREA, UPF), a researcher at the BCN MedTech Research Unit of the UPF Department of Engineering. The remaining researchers belong to different services and research groups of the Clínic-IDIBATS and are also linked to University of Barcelona and the CIBER for respiratory and rare diseases.
More than 200 pregnant women participated in the study
This research involved analysing fetal blood flow circulation and how it is altered when the mother receives extra oxygen, in the fetuses of 208 pregnant women at between 24 and 37 weeks of gestation. All of the women attended Hospital Clínic in Barcelona, where they underwent all the necessary tests for this study. In 97 of these cases, the fetuses had restricted growth, resulting in very low birth weight. The remaining 111 fetuses had normal growth. In each of these fetuses, the blood velocity of the main arteries and pulmonary vessels was measured, and then compared using AI. Additionally, the resistance of the lungs was calculated using a computer model.
The blood velocity in the lungs of the fetus was analysed both when the mother was breathing under normal conditions and after extra oxygen was delivered via a facemask (hyperoxygenation conditions). This analysis was carried out using a technique based on the emission of ultrasound waves to the fetus to estimate blood velocities throughout its circulation, based on Doppler principles.
In contrast, the resistance of organs, such as the lungs, cannot be measured directly with ultrasound, and a computer model representing the heart and blood vessels was used to measure it. To draw a parallel, we could compare this computer model to the simulation of an electronic circuit. The researchers recreated a computer version of the fetal vasculature and, using measured blood velocities and simulating the rest, they were able to estimate the resistance and elasticity of the different organs.
Finally, machine learning methods, based on artificial intelligence techniques, were used to compare blood flow patterns of the fetuses, thus aiding to group them into different categories according to flow and clinical parameters. When subsequently looking at the influence of hyperoxygenation, it was seen to be linked to changes in lung resistance, as a result of the extra oxygen delivered to the mothers, and it was shown that more oxygen improves blood flow in the lungs of fetuses with restricted growth, while having no influence in normal ones.
“Essentially, the research results indicate that in growth-restricted fetuses, the average blood velocity as well as vascular resistance in the lungs is different from normal fetuses, and that it can be normalized by supplying the mothers with extra oxygen” – explains Bart Bijnens (ICREA, UPF).
“The detection of these differences of the vessels of the lungs opens the door to the future design of therapeutic strategies to improve lung function in growth-restricted fetuses. After birth, these improvements in fetal development could reduce the risk of respiratory disease later in life”, explains doctor Fàtima Crispi (BCNatal, Clínic).
Reference article:
Vellvé, K., Garcia-Canadilla, P., Nogueira, M. et al. Pulmonary vascular reactivity in growth restricted fetuses using computational modelling and machine learning analysis of fetal Doppler waveforms. Sci Rep 14, 5919 (2024). https://doi.org/10.1038/s41598-024-54603-x
Journal
Scientific Reports
DOI
10.1038/s41598-024-54603-x
Method of Research
Experimental study
Subject of Research
People
Article Title
Pulmonary vascular reactivity in growth restricted fetuses using computational modelling and machine learning analysis of fetal Doppler waveforms
Article Publication Date
11-Mar-2024
What's Your Reaction?